blood glucose curve Oursler
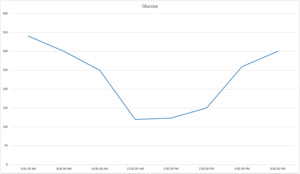
The results of a blood glucose curve. Photo by Dr. Teri Ann Oursler
After a few decades, people with unregulated (uncontrolled) diabetes tend to end up with retinal problems, blood vessel damage, kidney problems, etc. Because of their shorter life spans, dogs and cats with unregulated diabetes don’t usually face the same long-term consequences it causes in human diabetics. Normally their short life spans cause us grief, but in the case of a diabetic sometimes that short span can be a boon.
Pets who are unregulated diabetics will have symptoms that can be irritating, like urinating frequently (“I want in, I want out, I want in, I want out…oh hey, can I come in now?”) or urinating in inappropriate places, such as your new couch or your bedroom pillow. They also can have symptoms that threaten their health, like too much weight loss.
Our primary goal with diabetic dogs and cats is to give them a good quality of life: their body weight is stable, they don’t have to hover over the water dish all day, and their potty habits are normal in that they prefer to pee outside rather than on the couch.
Accurate monitoring of your pet's diabetes can help to maintain a good quality of life for both you and your pet. After all, who wants to curl up and watch a movie on a pee-soaked couch?
Exactly how does monitoring help us to accomplish this higher quality of life? By regulating their blood sugar (glucose) levels.
Normal blood glucose levels in dogs and cats are similar to those in humans, about 80-120 mg/dl (4.4-6.6 mmol/L). Animals whose blood glucose levels are in this range will look and act normal.
Fortunately for us, they will also act mostly normal if their blood glucose levels are as high as 100-250 mg/dl (5.5-13.75 mmol/L). We find that if we can maintain that level for as much of the day as possible, the pet will act pretty normal, with an acceptable amount of drinking and urinating (in the right places!), and stable body weight without becoming supermodel thin.
When the blood glucose levels are higher than 250 mg/dl (13.75 mmol/L), the kidneys are not able to keep the glucose from being lost in the urine; the glucose that is lost in the urine swoops water out with it, so the pet will drink a lot of water to keep up with what is being lost in the urine.
In general, that is our mission: keep the pet regulated so the kidneys can continue doing a happy dance while filtering out the stuff that needs to be removed. Nonetheless, we also have two other goals:
- To keep the dog or cat from having episodes of hypoglycemia (low blood glucose), which can lead to seizures and brain damage.
- To reverse diabetes in cats when possible. Within the first 6 months after diagnosis, we want to keep a cat’s blood glucose levels as close to normal (80-120 mg/dl (4.4-6.6 mmol/L) as possible, as most cats have type 2 diabetes. Because they still have their own insulin, if we take immediate steps to turn around the factors that are creating resistance to their own insulin, we can make their diabetes go away in about 70 percent of cats, like a genie stuffed back into the bottle, if the following steps are also taken:
- Reduce the cat's weight
- Switch to all-canned, low-carbohydrate diet
- Use an insulin that works well throughout the day
- Continue to aggressively monitor to keep their blood glucose levels as normal as possible.
Now we’re ready to talk about monitoring. There are several options used:
- A single blood glucose level
- A fructosamine level (a compound that reflects all the blood glucose levels that the dog or cat has had for the prior two to three weeks)
- The amount of glucose in the urine (which is measured on a dipstick as a color change and is estimated as 1+ for a low amount of glucose and 4+ for a large amount)
- Blood glucose curves, a series of blood glucose measurements done between the morning and evening insulin doses and meals.
What’s the difference between these methods? Why can’t we just do something simple, such as get a single blood draw for a fructosamine level or a single blood glucose level?
It’s like this: If we see a single high blood glucose level (say 350 mg/dl (19.25 mmol/L), or an elevated fructosamine level, it is human nature to interpret that in only one way: my pet needs more insulin.
However, we can see a high blood glucose or a high fructosamine level (or lots of glucose in the urine) when the pet is overdosed as well.
Yeah, that’s kind of confusing.
When blood glucose is too low, hormones such as cortisol and adrenalin rush right out of the cells to try to save the body from dying of low blood sugar. They do this, in part, by stopping the action of the injected insulin and causing the liver to release glucose. Thanks to these actions, however, the blood glucose swings wildly high in response to the injected insulin. If you measure the blood glucose levels later in the day, you’ll find them to be high. However, if you’ve only measured a single blood glucose at that time, you have no way of knowing that they’re high because there was too much insulin injected earlier in the day, or not enough insulin, so you’re inclined to give more, which just makes the problem worse.
Blood glucose curves are one way veterinarians can monitor your pet's diabetes. A blood glucose curve is a graph of blood glucose levels over time. This graph helps to establish the type, dose, and frequency of administration of insulin.
The other problem is that a single blood glucose or fructosamine level (the amount of glucose in the urine) tells us nothing about the kinetics of this insulin for this particular pet. Kinetics, meaning how this drug works in this individual animal, refer to how long the insulin lasts after each injection and how long it takes after each injection for the insulin to start working. You know, the small details that make the difference between a diabetic’s good day and a bad one.
Problems with kinetics can’t be fixed by changing the insulin dose: they can only be fixed by changing to a different kind of insulin, and the sooner we figure that out, the less time we waste trying to use an insulin that just doesn’t have the right kinetics for that particular pet.
So how do we do a blood glucose curve?
Because we’re trying to mimic what happens at home on a normal day, it’s best for the dog or cat to have their food and insulin injection at home the morning of the curve, then get dropped off at the veterinary hospital within an hour or so to start the curve.
Blood is collected every two hours throughout the day, changing to once-an-hour if the blood glucose levels are dropping to lower than 150 mg/dl (<8.75 mmol/), to ensure we don't miss an episode of potentially dangerous hypoglycemia.
Blood glucose curves can also be done at home, which can mean less stress for both owner and pet, and can result in a significant cost savings. It’s a good idea to get advice from your veterinarian about which glucometer brands are likely to be accurate. Some really are not accurate, and bad data is worse than no data.
Even a brand that tends to be reliable should be checked at the beginning for accuracy of that individual machine. To do that, have the first blood glucose curve done in the veterinary hospital, so they can check your glucometer against the hospital glucometer many times throughout the day’s curve.
Once it's established that your glucometer is reliably accurate, then they teach you how to collect the sample (the inside of the upper lip is an excellent site for dogs, using a lancet; in cats it's easiest to use the outer margin of the ears). Wherever the sample is collected, it is important not to ‘milk’ the site while trying to get a big-enough drop for the glucometer, because milking it to get a big-enough drop for the glucometer alters the blood glucose result and there is no reason to get bad data.
If you are generating the blood glucose curves in the comfort of your own home, so your dog can pee on the couch rather than in the car, it's important to share the results with your veterinarian. Your vet is trained to interpret it. Let your veterinarian make the decisions on adjusting the insulin dose for the sake of the couch and your pet.
While blood glucose curves are not foolproof, they give us the most accurate picture of how high and how low the blood glucose levels go during that day, how long the insulin is lasting, and how long it takes for the insulin to start working after each injection. Because the curves fluctuate from day-to-day, it is not possible to use one day’s curve to predict when to take a single blood glucose to ‘catch’ the lowest or highest blood glucose on a different day.
How often should a blood glucose curve be done? In a newly diagnosed diabetic, running a blood glucose curve once a week is recommended, then adjust the dose based on the results. It is important to wait a week after each dose change before running the next curve. Once the pet is regulated, then we can back off a bit and run the next curve in three months, or sooner if they develop symptoms of diabetes again (drinking too much, urinating too much, or losing weight).
In a newly diagnosed cat, however, where we're really hoping for the diabetes to go away, we run the blood glucose curves weekly while controlling the factors that cause insulin resistance. As the diabetes begins to resolve, the dose of insulin is decreased and decreased, until finally, the insulin can be stopped. We know cats in which the diabetes resolved within the first week of treatment with insulin and a canned low-carbohydrate diet, so careful monitoring is essential.
Blood glucose curves are best used as a more complete view of what THIS insulin is doing in THIS animal on THIS day. When that information is combined with the animal’s clinical picture ― how stable the body weight is, how much drinking and urinating is going on ― that helps us give your diabetic dog or cat, and your couch, the highest quality of life we can for as long as possible.
41 Comments
Sheri
October 26, 2022
Andrew P
March 22, 2022
Christy Corp-Minamiji, DVM
October 14, 2021
Kathy Wyler
October 6, 2012
Christy Corp-Minamiji, DVM
June 28, 2021
Nancy
June 27, 2021
Leonard W. Kolcz
June 24, 2021
Rebecca Padrick
June 17, 2021
Joe Cecchini
March 27, 2021
Deborah Jordan
February 15, 2021
Candice
January 24, 2021
Nancy Gibbons
January 4, 2021
Sarah Rosen
December 12, 2020
Paula C. Nolin
October 17, 2020
Stephanie Lardner
October 12, 2012
Christy Corp-Minamiji, DVM
October 5, 2020
Michele Adamski
September 29, 2020
Christy Corp-Minamiji, DVM
September 28, 2020
Sam Harper
September 26, 2020
Joanna
September 23, 2020
Colleen Whillans
August 15, 2020
Jackie
August 14, 2020
Robert
August 8, 2020
Angela G.
June 30, 2020
Beth DeVinney
June 15, 2020
Fran Munschauer
May 30, 2020
Hilary Rockwell
May 25, 2020
Christy Corp-Minamiji. DVM
March 22, 2020
Charlene Kendrick
March 22, 2020
Jennifer
March 6, 2020
Holly
January 18, 2020
Christy Corp-Minamiji, DVM
November 26, 2019
Z
November 24, 2019
Tani
October 27, 2019
Michelle Massotti
October 22, 2019
Christy Corp-Minamiji, DVM
September 11, 2019
Diana Gibbs
September 10, 2019
Deb Domurat
February 15, 2019
Gus Ray
May 30, 2018
Tania
April 14, 2017
Julia Dahlke
March 23, 2017
Kate McDuffee
March 23, 2017