Stem cell therapy transplants stem cells back into the body. Is it good for dogs?
Mesenchymal stem cells
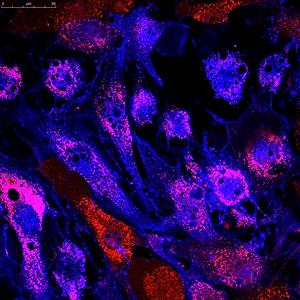
Mesenchymal stem cells labeled with fluorescent molecules. Photo courtesy of Depositphotos
“Shug, why are you limping?” I asked my dog as she bolted out the door after breakfast. It was barely noticeable. Still spry at 13 years young with no signs of slowing down, she refused to acknowledge the limp and within a couple minutes, it was gone. Years ago, I took x-rays of her hips and determined she had mild arthritis in both, one a little worse than the other. The limp hasn’t been back since.
I’m not against using non-steroidal anti-inflammatory drugs (NSAIDs) or other pain medications for my dogs, but due to her mild chronic kidney disease, I wasn’t ready to prescribe her anything stronger than a joint supplement. NSAIDs are commonly prescribed for dogs with arthritis pain but because they have the potential to affect the kidneys, it wasn’t a step I was ready to take.
Perusing the internet a couple days later, I searched, “osteoarthritis dogs therapies,” which yielded an article from a veterinary hospital that gave all the usual suggestions: physical therapy, physical conditioning, maintaining an optimum weight, and pain medications. That all sounded reasonable, but a note toward the bottom of the article mentioned stem cells as an option for dogs with joint disease. This surprised me. I first heard about stem cell therapy for pets about ten years ago, but I don’t know any veterinarians in my area offering or recommending it. I’ve never even had any meaningful conversations about the therapy with any of my colleagues.
I dug deeper. Reading an online report of a miraculous recovery in a dog who couldn’t walk before it had the therapy left me hesitant to believe. Resolving to get to the bottom of it, I tabled the report a result of a poorly researched news article. ‘Gimmicky’ comes to mind for any treatment labeled ‘a miracle’ until the result can be reliably reproduced in others and sufficiently tested for safety and efficacy.
What are stem cells? They aren’t just an aid for healing. They’re cells, when given the opportunity under the right conditions, that grow, replicate and mature into cells with a more specialized function, such as a muscle cell, a cartilage cell in a joint, etc. They offer potential in disease treatment because they have unique regenerative abilities and produce bioactive molecules that have effects on the immune system. Lots of researchers are looking at ways to manipulate these healing cells so that they will heal an injury or, for example, replace the insulin-producing cells in an individual affected by diabetes.
Stem cell therapy is the act of transplanting them back into the body. In many studies, researchers take fat out of the body and use an enzyme to break it down into a solution. Fat is a great source of a specific type of cell called mesenchymal stem cells (MSCs) because of its abundance and ease of collection. Other sources of stem cells include skin, blood, bone marrow, and muscle. Because they have the ability to divide and replicate, the cells will often be grown in flasks before being injected back into the patient. This process is also called passaging and is not always required before transplanting them.
After collecting and preparing the cells, they can be injected back into the same individual they were taken from, a process called an autologous transplant. Alternatively, the cells can come from a donor of the same species, which is called an allogenic transplant (e.g., from one dog to another or one person to another).
Significant advancements in human stem cell research have been made in recent years. Cells that restored vision with some diseases were authorized by the European Medicines Agency in 2015. In a clinical trial of stem cells combined with gene replacement therapy, 80% of defective skin was restored in a boy with junctional epidermolysis bullosa, a heritable blistering skin disease. But large-scale use for conditions like arthritis, heart disease, cirrhosis of the liver and such is still absent.
Stem cell therapy in people is years, perhaps decades, ahead of using it in veterinary patients where we haven’t yet convincingly demonstrated a benefit to our patients.
A recent, interesting study testing allogenic MSCs given by IV to dogs with skin allergies appeared to make a positive difference in the allergies. In this study, four dogs were prematurely withdrawn and excluded from the statistical analysis because they required additional medication to counteract their inflamed, itchy skin after treatment. Additionally, the scoring system used to rate improvements after patients received the therapy was not validated. While the results did appear to be promising, anticipating and eliminating issues like these should be a common goal for all future clinical studies.
Studies on arthritis in dogs have yielded positive findings, including improvement in lameness, pain, and range of motion. One study even reported lasting effects at a follow-up examination more than a year after the therapy.
While some of the results have been promising, results are often mixed and the threshold for the volume of data and positive effects needed to consider it an effective option have not yet been met. For example, studies in horses with joint disease have shown clinical improvement but failed to show comprehensive cartilage regeneration.
Without fully proving that it works, it’s merely a pipe dream, or worse, snake oil disguised by the peddler as a ‘miracle.’ Scientists still haven’t even figured out how they work. If we don’t know exactly how and why they’re working, we shouldn’t be offering them as treatment for our animals. They haven’t figured out the best or most effective way of delivering the stem cells. Should they be injected into the blood with the hope they can ‘home in’ on damaged tissue? Or should they be delivered into the target? Should we use the fat-derived mesenchymal cells? Or should we harvest stem cells from other tissues, like bone marrow? None of these questions have been answered yet.
For my patients and personal pets, when the time comes I’ll choose therapies I know will provide the promised effects, whether it be pain medications or a surgical procedure rather than a ‘hyped up’ therapy still in the experimental phase.
In the face of claims by companies promoting stem cell therapy for my patients, I’ve made up my mind to not recommend it. Despite what you may read, it hasn’t been proven safe or effective; studies attempting to prove its effectiveness are often riddled with problems complicating their interpretation such as small patient groups or lack of control groups. To justify veterinarians recommending it, we need more studies telling us, without doubt, it provides clinical benefit. Often the studies we have are strictly proof of concept, yield positive findings that are not repeatable, or were only performed in laboratories and have yet to be validated in actual patients.
Sadly, the therapy is currently being offered for pet diseases. Due to the absence of actual evidence to support effectiveness and safety, this just isn’t ethical. The International Society for Cell and Gene Therapy has raised concerns about unproven cell therapies harming human patients as well as the long history of profits and abuse from the marketing of unproven medical interventions, which extends to veterinary medicine.
Let’s treat our furry companions with more regard by demanding only the best: scientifically proven and ethical treatments. They are amongst our most loyal friends, after all.
Whichever way you frame it, we aren’t there yet. Just because the option for stem cell therapy exists doesn’t mean it’s a good one.
2 Comments
Nathan Mueller, DVM, MS
January 22, 2021
Larry Snyder, DVM, MS
January 12, 2021