Introduction
Disseminated intravascular coagulation (DIC) is an acquired life threatening disorder that results in loss of localized regulation leading to widespread systemic activation of coagulation. It is not a primary disease but rather a secondary process that leads to pathologic activation of the extrinsic and/or intrinsic coagulation pathways. It can be initiated by a number of underlying conditions and is a dynamic process that varies clinically from mild alterations in laboratory parameters to more common severe forms associated with microthrombosis and/or severe diffuse bleeding and multiorgan failure. It is commonly reported in dogs and less commonly identified in cats.
In DIC the normal localized hemostatic mechanisms regulating coagulation are disrupted leading to activation of coagulation with excessive fibrin and clot formation (resulting in microthrombi of small to medium sized vessels in organs throughout the body and multiorgan failure), consumption of clotting factors/platelets and in some cases activation of fibrinolysis (leading to excessive bleeding). Either or both microthrombi and bleeding may be present to different degrees in different patients leading to a myriad of clinical signs and laboratory abnormalities. Depending on the underlying mechanism that activates the coagulation systemically, the rate of activation and the body's compensation, DIC may present as an acute fulminant condition or a low-grade chronic condition with no obvious clinical thrombosis or hemorrhage.
Underlying Conditions
A number of underlying conditions have been associated with DIC, particularly infectious causes and those associated with SIRS. These include bacterial, viral, protozoal, and fungal infections as well as massive tissue trauma, shock, heat stroke, pancreatitis, severe burns, snake and insect envenomation, gastric dilatation and volvulus, severe gastrointestinal diseases, heart worm, immune mediated diseases and transfusion reactions. Malignancies are also a common cause of DIC in dogs. In cats the most commonly reported conditions include neoplasia, pancreatitis, and sepsis.
The Role of Inflammation in DIC
DIC is most commonly associated with underlying diseases that cause a systemic inflammatory response syndrome (SIRS) and sepsis. There is cross talk between the coagulation system and inflammation with the initiation of coagulation influencing inflammation and the presence of inflammation activating coagulation. In essence a viscous cycle between inflammation and coagulation exists that initiates and propagates DIC. There are essentially two main mechanisms that result in sufficient inflammation to initiate systemic coagulation: 1) release or expression of tissue factor (activation of extrinsic pathway of coagulation), and 2) widespread injury to endothelial cells exposing subendothelial collagen (aggregation and activation of platelets) and tissue factor (activation extrinsic pathway of coagulation).
Depending on the underlying cause there may be more than one mechanism initiating systemic activation of coagulation, although the processes are often interrelated (see Figure 1). For example with gram-negative bacterial infections endotoxins can cause direct endothelial injury (exposure of subendothelial collagen and tissue factor) and inhibit thrombomodulin (which has anticoagulant properties), or through stimulation of cytokines (particularly TNF alpha and IL1) by immune cells, cause increased expression of tissue factor on inflammatory cells (monocytes) and endothelial cells (extrinsic pathway activation) and direct activation of factor XII (intrinsic pathway activation). In massive trauma the major trigger is the release of tissue factor into circulation (extrinsic pathway activation). In obstetric conditions tissue factor derived from the placenta, dead retained fetus, or amniotic fluid may enter the circulation. In the case of neoplasia some cancer cells constitutively express high levels of tissue factor promoting initiation of DIC. With certain envenomation's clotting factors may be directly activated by the venom or its metabolites.
| Figure 1. Pathophysiology of DIC | 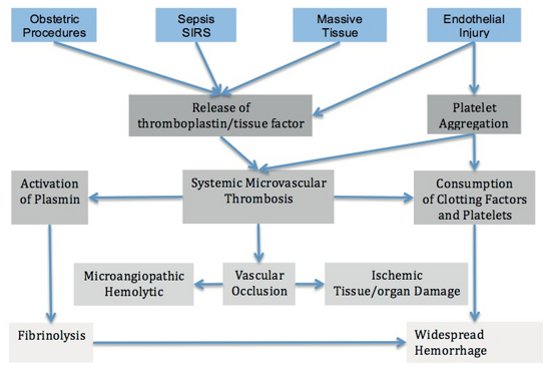
|
|
| |
Clinical Manifestations of DIC
DIC generally results in two main sequelae:
1. Systemic deposition of fibrin within the microcirculation leading to ischemia (when severe) and microangiopathic hemolytic anemia (as red cells are fragmented when they try to squeeze through narrowed microvasculature).
2. Consumption of platelets and clotting factors, and activation of plasminogen (which results in fibrinolysis) which lead to widespread hemorrhage.
Given it is a secondary process and the complexity and multifactorial nature of DIC it is impossible to predict the clinical signs that will be seen in all forms of DIC. However, the findings of microangiopathic hemolytic anemia, unexplained dyspnea, bleeding/oozing from surgical incisions/catheter sites, and sudden progressive circulatory failure and shock should prompt consideration of DIC.
Prognosis
Due its complex dynamic nature DIC tends to be challenging to diagnose and treat carrying a grave prognosis. Veterinary studies report mortality rates in dogs with DIC as ranging from 50–77%, while the mortality rate in cats is as high as 93%.
References
1. Bruchim Y, Aroch I, Saragusty J. Disseminated intravascular coagulation. Compend Contin Educ Vet. 2008;30(10):E1–E16.
2. Stokol T. Disseminated intravascular coagulation. In: Weiss, Wardrop, eds. Shalm's Veterinary Hematology. 6th edition. Ames, IA: Wiley Blackwell; 2010.