Professor, Internal Medicine, Dept. Small Animal Medicine, Ghent University
Merelbeke, Belgium
The choice of therapy for hypercortisolism depends on the localisation of the problem (adrenal versus pituitary tumor), the availability of more sophisticated methods (hypophysectomy and radiation therapy), motivation and budget of the owner and experience of the veterinarian. This lecture will focus on current treatment options of pituitary dependant hypercortisolism (PDH).
When available, transsphenoidal hypophysectomy (surgical removal of the whole pituitary gland) is the treatment of choice for many dogs with PDH. Indeed, this surgery aims for the removal of the cause of the disease. Currently this can be performed at the University clinic of Utrecht, The Netherlands. Travel and cost are the limiting factors. The prognosis for dogs treated with hypophysectomy is good if the diagnosis of PDH is made early and the pituitary gland is only mildly to moderately enlarged. For macrotumors the prognosis is not that good. Many dogs require vasopressin supplementation during the post operative period, and all dogs require a life-long therapy with cortisone and L-thyroxine.
Until recently, chemotherapy with o,p'-DDD (Lysodren® or Mitotane®) was used to treat most dogs with PDH. This drug causes a destruction of the adrenal cortex. Two protocols have been described: selective (partial) or non-selective (complete) destruction of the adrenal cortex. The adrenal cortex is formed by 3 layers, the zona fasciculata, zona reticularis (secretes glucocorticoids and androgens), and the zona glomerulosa (produces only mineralocorticoids). This is a lypophilic drug and therefore always needs to be administered with food. Furthermore, gloves need to be worn when manipulating this drug. o,p'-DDD should not be administered when the patient is or becomes anorectic.
The selective protocol consists of an induction period of approximately 7 days and is followed by a life-long maintenance therapy with Lysodren®. The protocol aims at a selective destruction of the adrenal cortex sparing the zona glomerulosa and decreasing cortisol secretion.
With the non-selective protocol (Utrecht protocol), a high dosage of Lysodren® is administered during a limited period. This protocol aims at a complete destruction of the adrenal cortex (zona fasciculata, zona reticularis and zona glomerulosa). Hypocortisolism and hypoaldosteronism will ensue. A life-long therapy with glucocorticoids and mineralocorticoids is mandatory.
Trilostane (Vetoryl®) has been used with success to treat dogs with PDH since 1997. Initially, the veterinary preparation was only available in England. Recently it has become widely available throughout Europe. Trilostane is a synthetic steroid with no inherent hormonal activity. It is a competitive inhibitor of the 3-β-hydroxysteroid-dehydrogenase enzyme system. Hence, Trilostane blocks the adrenal synthesis of glucocorticoids, sex hormones and to a lesser extend mineralocorticoids.
Recently, a consensus meeting (Amsterdam, April 19th, 2006) recommended a relatively low starting dose of Trilostane of 2.5 mg/kg per os, once daily. It is our experience that, especially in small dogs, this dosage will limit side effects. Only capsules of 30 and 60 mg are available, which can be problematic for small dogs. Reformulating the capsule (when country legislation allows it) is an option in small dogs to allow more optimal dosaging.
Close monitoring of Trilostane therapy is required. Decreased polyuria/polydipsia/polyphagia and increased activity are already often reported by the owners at the first control visit (7-14 days after initiation of therapy). Dermatological improvement will only occur later. Dosage adjustments are based on the clinical improvement, electrolyte measurements and monitoring of the adrenal reserve. The latter is performed with an ACTH stimulation test, which is best performed 2-3 hours after Trilostane administration. Indeed, the effects of Trilostane last for only a few hours. Initial dosage adjustments are required in most dogs. These are often made in increments of 10-30 mg per dog. Once the goal of therapy is achieved (good clinical control with post ACTH cortisol level between 40 and 150 nmol/L), check up is planned every 3 months. Most dogs tolerate the treatment with Trilostane well, especially when the therapy is started with a conservative dosage (2.5 mg/kg). The effective dosage of Trilostane varies largely among dogs. Exceptionally, dosages of 15 mg/kg or more need to be administered.
Possible side effects include vomiting, diarrhoea and lethargy. These can be self-limiting or require cessation of therapy. Rarely, hypoadrenocorticism develops and needs to be treated. This is confirmed by an ACTH stimulation test (absence of increase in cortisol after ACTH administration).
Noteworthy are the ultrasonographic changes of the adrenal cortices (increased thickness and echogenicity) reported during Trilostane therapy. These changes are due to increased ACTH levels resulting from the diminished negative feed back normally exerted by cortisol.
A study from Barker et al. showed that survival times between dogs treated with Trilostane and those treated with Mitotane® were not significantly different (median of 662 and 708, respectively).
Because of their limited efficacy and/or potential side effects, the use of ketoconazol and L-deprenyl will not be discussed.
Approximately 20 % of dogs with PDH develop neurological signs because of dorsal expansion of the pituitary tumor. Therefore, in dogs with PDH, medical imaging of the pituitary gland (CT scan or MRI) should be recommended to the owners. If a large pituitary tumor is detected, with or without neurological signs, radiation therapy is indicated. Indeed, pituitary tumors are relatively sensitive to radiation. The aim here is to decrease the volume of the space occupying pituitary mass. Dogs may already show some improvement (i.e., improved alertness in a dull dog) during radiotherapy but improvement is often delayed. Most often the treatment has no or little effect on the hormonal secretion of the tumor. Therefore, medical therapy is still warranted and most often started 1-3 weeks after termination of the radiation therapy.
Prognosis for PDH with appropriate treatment and monitoring is favorable in many dogs. However, treatment of PDH requires a major commitment by the owner and the veterinarian.
Click on the image to see a larger view
| Figure 1. | 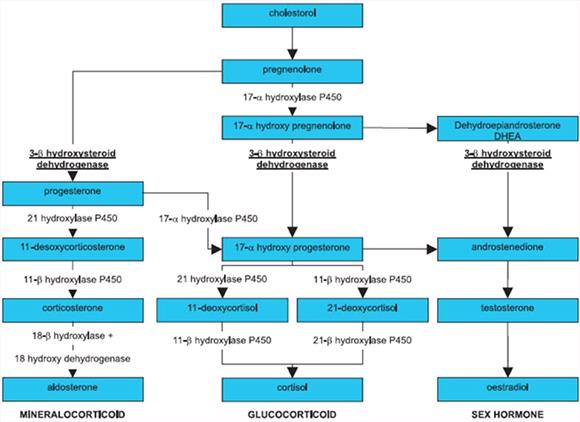
Schematic representation of the adrenal steroid biosynthesis. Trilostane inhibits the action of the 3β-hydroxysteroid-dehydrogenase enzyme in the adrenal cortex. |
|
| |
References
1. Barker EN, Campbell S, Tebb AJ, Neiger R, Herrtage ME, Reid SWJ, Ramsey IK. A comparison of the survival times of dogs treated with mitotane or trilostane for pituitary-dependent hyperadrenocorticism. Journal of Veterinary Internal Medicine 2005; 19: 810-815.
2. British Small Animal Veterinary Association Manual of Canine and Feline Endocrinology. 3rd edition. Edited by CT Mooney and ME Peterson. ME Herrtage. Canine hyperadrenocorticism. P. 150-172.
3. Hanson JM, van't Hoofd MM, Voorhout G, Teske E, Kooistra HS, Meij BP.Efficacy of transsphenoidal hypophysectomy in treatment of dogs with pituitary-dependent hyperadrenocorticism. Journal of Veterinary Internal Medicine 2005; 19: 687-694.
4. Neiger R, Ramsey I, O'Connor J, Hurley KJ, Mooney CT. Trilostane treatment of 78 dogs with pituitary-dependent hyperadrenocorticism. Veterinary Record 2002; 150: 799-804.
5. Ruckstuhl NS, Nett CS, Reusch CE. Results of clinical examinations, laboratory tests, and ultrasonography in dogs with pituitary-dependent hyperadrenocorticism treated with trilostane. American Journal of Veterinary Research 2002; 63: 506-512.
6. Wenger M, Sieber-Ruckstuhl NS, Muller C, Reusch CE. Effect of trilostane on serum concentrations of aldosterone, cortisol, and potassium in dogs with pituitary-dependent hyperadrenocorticism. American Journal of Veterinary Research 2004; 65: 1245-1250.