Kit Sturgess, MA, VetMB, PhD, CertVR, DSAM, CertVC, MRCVS, RCVS Recognised Specialist in Small Animal Medicine
Making the Diagnosis and Getting the Treatment Right
This presentation will focus on decision making in diagnosis in cases of gastrointestinal tract (GIT) disease in cats. GIT disease is a common presenting problem but often will have subtle signs as many cats go outside to defecate and are fastidious about grooming. Hence diarrhoea or vomiting, if present, may not be obvious. In around 10-20% of cats, GIT disease presents as weight loss often associated with appetite change as the only clinical signs. Appetite changes can include both anorexia and polyphagia; some cats go through cycles with marked variation in appetite.
Is the Problem Likely to be Self Limiting?
Many acute episodes of vomiting and diarrhoea will be self limiting and do not require significant investigation. The key decisions in such cases are:
1. Does this case fit the criteria to be a short-term, self limiting problem?
2. What symptomatic therapy can I use that will not interfere with further investigation should the case turn out to be non-self limiting?
Cases that are likely to be self limiting:
 History is short
History is short
 Known exciting cause, e.g., change of diet
Known exciting cause, e.g., change of diet
 Cat is systemically well
Cat is systemically well
 Negative physical findings
Negative physical findings
 Appetite remains good
Appetite remains good
Symptomatic Therapy
|
Therapy that is unlikely to worsen or prolong clinical signs or interfere with further investigation |
Therapy that may worsen or prolong the clinical signs and/or interfere with further investigation |
Therapy that will interfere with further investigation |
|
Starvation |
Antimicrobials |
Corticosteroids |
|
Bland diet |
Atropine |
|
|
Mucosal protectants e.g., sucralfate, kaolin |
Non-steroidal anti-inflammatory drugs |
|
|
Antacids e.g., magnesium hydroxide, H2-blockers |
Anti-emetics and prokinetics e.g., metoclopramide, cisapride |
|
|
Vitamin supplementation |
|
|
Problem Is Not Self Limiting
A. Acute With Systemically Unwell Cat
History
Should be used to localise disease as far as possible and assess severity, duration and progression of signs; evidence of other disease; nature, frequency and timing of vomiting/diarrhoea; appetite and attitude to food.
 Non-gastrointestinal disease with gastrointestinal signs
Non-gastrointestinal disease with gastrointestinal signs
 Oral disease:
Oral disease:
 Inappetence
Inappetence
 Dysphagia
Dysphagia
 Pain
Pain
 Halitosis
Halitosis
 Oesophageal vs. gastric/small intestinal:
Oesophageal vs. gastric/small intestinal:
 Vomiting vs. regurgitation
Vomiting vs. regurgitation
 Recent anaesthesia or medication
Recent anaesthesia or medication
 Upper gastrointestinal tract:
Upper gastrointestinal tract:
 Vomiting
Vomiting
 Diarrhoea
Diarrhoea
 Inappetence
Inappetence
 Weight loss
Weight loss
 Colonic disease--rarely systemically ill, history tends to be chronic:
Colonic disease--rarely systemically ill, history tends to be chronic:
 Dyschezia
Dyschezia
 Haematochezia
Haematochezia
 Tenesmus
Tenesmus
 Constipation
Constipation
Full Physical Examination
The emphasis should be towards prioritizing further investigation and therapeutics. Check level of dehydration; evidence of blood loss, pleural or peritoneal fluid, aspiration or mediastinitis, obstruction; evidence of peritonitis, pain.
Further Investigation and Therapeutics
Directed towards management of pain, dehydration and sepsis; control of vomiting and nutritional needs.
Diagnostics
Decisions should be based on safety/invasiveness and the likelihood of delivering useful clinical information on which treatment can be based.
 Haematology and biochemistry including electrolytes
Haematology and biochemistry including electrolytes
 FeLV/FIV / coronavirus (?) serology
FeLV/FIV / coronavirus (?) serology
 Thoracic and abdominal radiographs
Thoracic and abdominal radiographs
 Abdominal ultrasound
Abdominal ultrasound
 (Endoscopy)
(Endoscopy)
 Exploratory surgery--planning is important. 'If I find ....... what will I do/change therapeutically?'
Exploratory surgery--planning is important. 'If I find ....... what will I do/change therapeutically?'
B. Chronic and Recurrent
In most cases of chronic GIT disease there is time to conduct a stepwise and logical investigation. Necessary diagnostics should be conducted before therapeutic interventions that could make interpretation of results difficult.
History
Common signs suggestive of gastrointestinal disease include anorexia, diarrhoea, polyphagia, vomiting, weight loss.
Less common signs are abdominal enlargement, pallor, jaundice, ptyalism, regurgitation, tenesmus, dyschezia and haematochezia, weakness and lethargy.
Physical Examination
Physical examination in chronic GIT disease is often unrewarding. However, attention should be paid to the oral cavity (evidence of dental disease, gingivitis, pallor), superficial lymph nodes, thyroid gland, presence of enlarged abdominal lymph nodes, thickness of the small intestine, amount of faeces in the colon, abdominal pain / discomfort.
Diagnostic Investigation
Test selection is affected by clinical signs. The list below is not exhaustive but provides a general diagnostic route.
Initial Investigation
1. Faecal analysis:
a. Selective culture--Salmonella and Campylobacter, Clostridia.
b. Parasitology including flotation for Giardia, Cryptosporidia, Tritrichomonas foetus.
c. There is no evidence that non-selective culture looking at relative levels of other bacteria such as E.coli has any association to clinical disease.
d. Pathogenic E.coli may be of some importance but current tests show similar levels of toxigenic E.coli in cats with and without diarrhoea.
2. Routine haematology, biochemistry and endocrine testing: Usually a low yield procedure but may be of value to exclude some systemic causes, intercurrent disease and assess whether there may be anaemia associated with GIT haemorrhage, hypoproteinaemia or changes in liver parameters. Test for hyperthyroidism in older cats and (rarely) hypoadrenocorticism.
3. Urinalysis: Can be of value especially in cases with weight loss, raised urea/creatinine or hypoalbuminaemia.
Secondary Investigation
1. Examination of oral cavity ± dental radiographs under general anaesthetic: This is important in cats showing anorexia and weight loss in the absence of other clinical signs to explain it. It is also important if a linear foreign body is suspected.
2. Diagnostic imaging: Relatively low yield procedure but will help to exclude masses not felt on physical examination, localised peritonitis. Abdominal ultrasound can be used to demonstrate normal layering (Figure 1) and thickness (< 3.5 mm) of small intestine and stomach, pancreatic or hepatic disease, prominence of mesenteric lymph nodes. Ultrasound is the most sensitive method to exclude small volume peritoneal effusions.
3. Ultrasound can be of value in defining regional abnormalities that may direct future investigation, particularly whether endoscopic biopsies or full thickness biopsies would be the more appropriate.
4. Cobalamin (B12) and folate: The value of measuring these parameters has not been well demonstrated in cats in terms of diagnosis. Low cobalamin levels have been associated with poor response to treatment regardless of cause.
5. Feline TLI (fTLI): Highly sensitive in diagnosis of exocrine pancreatic insufficiency (EPI) but specificity may be poor. EPI is rare in cats. Elevation above the reference range to assess pancreatic inflammation is controversial. It is most likely to have a low sensitivity and specificity.
6. Feline pancreatic lipase (fPLi): This is an isoenzyme specific immunoreactivity test. Currently only performed in the USA but likely to become more widely available both as a patient-side and external laboratory test. Evidence suggests that it is the most sensitive and specific test available, apart from biopsy, to demonstrate pancreatitis. Sensitivity in the diagnosis of chronic, grumbling pancreatitis compared to acute or active pancreatitis.
| Figure 1. Normal intestinal layering. | 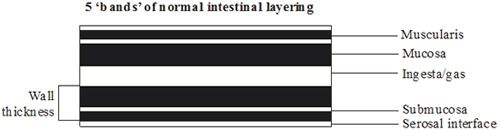
|
|
| |
Tertiary Investigation
1. Biopsy and histopathology:
Decision as to which is the most appropriate technique is based on
a. Results of previous tests
b. Tissue samples required
c. Equipment availability
d. Expertise
e. Risk
f. Costs
g. Likely diagnosis and treatment
h. Post operative complications following full thickness biopsies can be high. In some studies, endoscopic biopsies have low sensitivity for detecting lymphoma.
2. Other tests: Duodenal juice culture, breath hydrogen testing and differential sugar absorption are all described in the cat. Their clinical utility remains low.
Alternatives to Corticosteroids in the Management of Inflammatory Bowel Disease
Therapeutic decisions depend on clinical signs, results of diagnostic tests, pathology reports, evidence of intercurrent disease and owner preferences.
Risks Associated with Using Corticosteroids
Table 2. Disadvantages of glucocorticoids.
|
Specific contraindications |
Potential side effects |
|
 Infections--may exacerbate bacterial, viral and fungal infections both via immunosuppression particularly where a cell mediated response is important and may promote viral replication. Particularly feline poxvirus, herpes and calicivirus infections Infections--may exacerbate bacterial, viral and fungal infections both via immunosuppression particularly where a cell mediated response is important and may promote viral replication. Particularly feline poxvirus, herpes and calicivirus infections
|
 Polyphagia and weight gain Polyphagia and weight gain
 Polyuria / polydipsia Polyuria / polydipsia
 Dermatologic changes--lacking of hair regrowth, thinning of skin, comedones, fragile skin syndrome, medial curling of ear tips Dermatologic changes--lacking of hair regrowth, thinning of skin, comedones, fragile skin syndrome, medial curling of ear tips
|
|
 Demodicosis Demodicosis
|
 Immunosuppression, lymphoid atrophy Immunosuppression, lymphoid atrophy
|
|
 Renal disease (increase in nitrogenous waste from catabolic effects and tendency to cause hypertension and worsen proteinuria) Renal disease (increase in nitrogenous waste from catabolic effects and tendency to cause hypertension and worsen proteinuria)
|
 Mood changes--depression, euphoria Mood changes--depression, euphoria
 Lethargy Lethargy
 Hypertension Hypertension
|
|
 Cardiovascular disease (sodium retention with subsequent plasma volume expansion) Cardiovascular disease (sodium retention with subsequent plasma volume expansion)
|
 Gastrointestinal ulceration (especially if concurrent NSAID use) Gastrointestinal ulceration (especially if concurrent NSAID use)
|
|
 Pregnant queens (induce foetal adrenocortical atrophy and can be teratogenic and abortifacient) Pregnant queens (induce foetal adrenocortical atrophy and can be teratogenic and abortifacient)
|
 Steroid hepatopathy--predisposition to hepatic lipidosis Steroid hepatopathy--predisposition to hepatic lipidosis
 Pancreatitis Pancreatitis
|
|
 Kittens (suppress growth hormone and somatostatin mediated osteoblast function) Kittens (suppress growth hormone and somatostatin mediated osteoblast function)
|
 Redistribution of body fat Redistribution of body fat
 Tachypnoea & panting Tachypnoea & panting
|
|
 Diabetes mellitus (gluconeogenic and insulin antagonistic) Diabetes mellitus (gluconeogenic and insulin antagonistic)
|
 Insulin resistance Insulin resistance
 Growth retardation Growth retardation
|
|
 Corneal ulceration (delay healing and increases the risk of perforation) Corneal ulceration (delay healing and increases the risk of perforation)
 Gastrointestinal ulceration Gastrointestinal ulceration
|
 Decreased muscle mass & muscle weakness Decreased muscle mass & muscle weakness
 Reduced fibroblast activity and wound healing Reduced fibroblast activity and wound healing
|
|
 ? pancreatitis ? pancreatitis
 ? amyloidosis ? amyloidosis
|
 Iatrogenic hypoadrenocorticism (withdrawal syndromes) Iatrogenic hypoadrenocorticism (withdrawal syndromes)
|
|
|
 Osteoporosis Osteoporosis
|
Alternatives to Consider
Diet
Essential part of IBD therapy. Good owner and cat compliance is crucial, meaning feeding the diet to exclusion for 2 weeks.
 Hydrolysed dry diets (chicken or soya) that potentially have reduced immunogenicity. If not truly hypoallergenic, these diets are certainly novel proteins. Acceptance is variable--some cats will vomit on such diets.
Hydrolysed dry diets (chicken or soya) that potentially have reduced immunogenicity. If not truly hypoallergenic, these diets are certainly novel proteins. Acceptance is variable--some cats will vomit on such diets.
 Novel, single source, protein diets that are highly digestible, low fat and gluten free--available dry and wet.
Novel, single source, protein diets that are highly digestible, low fat and gluten free--available dry and wet.
 Home cooked.
Home cooked.
Cobalamin (B12)
Cats that are cobalamin-deficient have been shown to have a poorer response to other treatments.
Dose: 20 μg/kg s/c weekly for 4 weeks.
Antacids, Mucosal Protectants, Anti-emetics and Prokinetics
Consider where vomiting is a major feature especially if inflammation is primarily confined to the stomach, and therefore may be secondary to the vomiting.
 Mucosal protectant:
Mucosal protectant:
 Sucralfate: 50-100 mg/kg TID PO one hour before feeding and not with other drugs
Sucralfate: 50-100 mg/kg TID PO one hour before feeding and not with other drugs
 H2-blockers:
H2-blockers:
 Cimetidine: 5-10 mg/kg TID PO
Cimetidine: 5-10 mg/kg TID PO
 Ranitidine: 3.5 mg/kg BID PO
Ranitidine: 3.5 mg/kg BID PO
 Famotidine: 1 mg/kg SID-BID PO
Famotidine: 1 mg/kg SID-BID PO
 Proton pump inhibitors:
Proton pump inhibitors:
 Omeprazole: 0.7 mg/kg SID PO
Omeprazole: 0.7 mg/kg SID PO
 Anti-emetics and prokinetics:
Anti-emetics and prokinetics:
 Metoclopramide: 0.2-.5 mg/kg TID/QID PO
Metoclopramide: 0.2-.5 mg/kg TID/QID PO
 Cisapride: 2.5 mg/cat BID
Cisapride: 2.5 mg/cat BID
 Prochlorperazine (Stemitil): 0.5-1 mg/kg BID-TID PO or PR
Prochlorperazine (Stemitil): 0.5-1 mg/kg BID-TID PO or PR
Helicobacter Treatment
Although Helicobacter is present in virtually all cats, consider treatment if inflammation is mild to moderate and confined to the stomach.
 Amoxicillin 10-20 mg/kg BID
Amoxicillin 10-20 mg/kg BID
 Metronidazole 10 mg/kg BID
Metronidazole 10 mg/kg BID
 Antacid
Antacid
Metronidazole and Doxycycline
Appear to be very useful drugs in the management of inflammatory bowel disease. Their modes of action are unclear but probably a combination of control of bacterial numbers and immunomodulation. With diet it is my first choice medication for mild IBD.
 Giardia not excluded--metronidazole 20 mg/kg BID for 5 days then 10 mg/kg BID for 25 days
Giardia not excluded--metronidazole 20 mg/kg BID for 5 days then 10 mg/kg BID for 25 days
 Giardia excluded--metronidazole 10 mg/kg BID for 30 days
Giardia excluded--metronidazole 10 mg/kg BID for 30 days
 Doxycycline--10 mg/kg SID with water
Doxycycline--10 mg/kg SID with water
Cyclosporine (Ciclosporin)
Neoral is the preferred preparation as it is becomes a microemulsion on contact with gastrointestinal fluids and thus has improved absorption. It should be given twice daily; trough serum levels of 250-500 ng/ml are recommended. This can usually be achieved at dose rates of 1-5 mg/kg BID. Nephrotoxicity and hepatotoxicity are low. Very high plasma levels may lead to anorexia and opportunistic fungal and bacterial infections. Acute toxoplasmosis has been described. FeLV and FIV status should be checked before initiating therapy. Cyclosporine has an unpleasant taste and the oral solution is better placed in an empty gelatin capsule. If the volume required is very small, dilution with olive oil allows accurate dosing and is stable.
Atopica (Novartis Animal Health) is available as 10 mg and 25 mg capsules.
Chlorambucil
First choice drug in severe IBD or mature lymphocytic lymphoma. Major side effect is immunosuppression so monitoring of haematology is required.
Dose: 2-4 mg/m2 EOD PO but requires tablet division; or 15 mg/m2for 4 consecutive days every 3 weeks.
Cyclophosphamide
Has been used at immunosuppressive dose rates in severe, non-responsive IBD. Side effects are perhaps more frequent than chlorambucil--profound marrow suppression and haemorrhagic cystitis.
Dose: 50 mg every 6-8 days.
Other Forms of Corticosteroids
 Enemas
Enemas
 Budesonide--some steroids such as budesonide show considerable first pass metabolism and have less systemic side effects; they can be used orally to treat intestinal disease. Dose rate--3 mg/m2/day.
Budesonide--some steroids such as budesonide show considerable first pass metabolism and have less systemic side effects; they can be used orally to treat intestinal disease. Dose rate--3 mg/m2/day.
References
References are available upon request.