illustration of dog with tetanus
Extremely affected dogs show rigidity in every muscle, even the ears. Classically there is a history of a wound in a tetanus case (generally in the preceding 1-2 weeks) but sometimes the wound has gone unnoticed by the owner and this important clue is not available. Graphic by MarVistaVet
We have all heard of tetanus shots and have some sense that we are supposed to periodically get them, especially after exposure to some sort of dirty wound or bite. Some of us may even know that tetanus is sometimes referred to as lock jaw, but the general knowledge of tetanus generally does not extend much beyond that. Unless you work with livestock, you may not realize that tetanus is a concern for animals as well as for people. Tetanus is a disease caused by a toxin secreted by a bacterium known as Clostridium tetani, one of many toxin-secreting Clostridia. These bacteria are anaerobic, meaning that they grow in conditions where there is no oxygen (such as a deep bite wound or puncture). Clostridia are soil bacteria, meaning that they live in dirt so it should be easy to see how a puncture contaminated with dirt would be a classical tetanus-yielding wound. Such wounds are particularly common on farms where there might be nails or bits of wire on the ground, ready to pierce a human or animal foot, but there is nothing special about rusted metal in predisposing to tetanus. The puncture can come from any pointed object. The pointy object provides the puncture (an anaerobic wound) and contamination with dirt provides the Clostridia. A fight involving a bite wound and rolling around in dirt might similarly offer an opportunity for tetanus.
Different animal species have different sensitivity to the tetanus toxin. Horses, humans, and livestock are more sensitive while cats are quite resistant and almost never get infected. We will be confining our discussion primarily to dogs.
The Course of the Disease
The tetanus toxin is called tetanospasmin. It is produced by the bacterium Clostridium tetani in a wound. The toxin binds to local nerves and migrates up into the central nervous system where it interferes with the release of glycine and GABA, both of which are inhibitory neurotransmitters. The result of this loss of inhibition is painful muscle over-activity, spasms and rigidity. In severe cases, the patient cannot breathe because of the rigid paralysis of the respiratory muscles and a mechanical ventilator is required. As a human disease, tetanus has been known and described since ancient times. In the modern world, human death is unusual and is mostly limited to infants and to the elderly, but even in these groups mortality is only 10-15 percent.
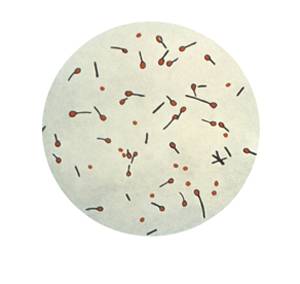
Cultured Clostridium tetani spores. Photo by CDC
The incubation period of tetanus is 3 to 21 days, with 5 to 10 days from the original wound being more typical. Classically, the patient first loses the ability to blink and must flash the third eyelid to moisten the eye. The patient becomes sensitive to light and sound such that clapping one’s hands can actually create spasms or seizures. Dogs with ears that hang down may actually develop ears that stand up straight, and the facial muscles pull back in such a way as to create what is called the risus sardonicus or sardonic smile. In more advanced stages, the patient can no longer walk and stands stiffly in what is called a sawhorse stance. In an advanced state of disease, the patient cannot walk or even sit up and is at risk for aspiration of saliva or food contents. If the jaws are locked, feeding may be impossible and if the respiratory muscles become involved, the patient will not be able to effectively breathe.
In dogs, a localized tetanus is more common than the generalized (whole body form) and only the limb nearest the original wound becomes rigid or will tremor. This is an easier form to treat compared to the more generalized; however, the localized form can spread and become the generalized form.
In the generalized form, initial signs seem to pertain to the eyes and can easily be mistaken for eye disease in the early stages.
Testing
There is no test for tetanus in the way you might hope: no blood test or unique finding. The diagnosis is generally made based on the appearance of the animal and history of a wound. It is possible to measure antibody levels against the tetanus toxin but this has not been widely used in the clinical setting. Attempting to culture Clostridium tetani from the wound is generally not successful.
Therapy
The first step in treatment is antibiotics to kill the Clostridia. Happily, unusual antibiotics are not needed: penicillin works quite well for this classical gram positive rod. Clindamycin and metronidazole are also felt to be effective. Improvement is usually obvious in the first week of treatment.
Sedation is necessary to control the spasms and/or seizures. Acepromazine and chlorpromazine have been recommended to control the sensitivity to light and noise. The patient will need a darkened quiet room and may need his eyes covered to reduce stimulation. These medications can promote seizures in other sets of circumstances, but tetanus is the exception. Injectable pentobarbital, phenobarbital, propofol, methocarbamol, diazepam, or midazolam can be used to control the muscles stiffness.
Patients for whom respiratory compromise is a concern (when the respiratory muscles are affected or if there is larynx spasm) may actually need days of general anesthesia, an endotracheal tube (tube in the windpipe to keep an airway open) or even a mechanical ventilator.
The decision on whether or not to include tetanus antitoxin is more controversial. Antitoxin is an antibody solution (a blood product) generated by either a horse or human to bind and destroy the tetanus toxin. It cannot remove toxin already bound to the patient’s nerves but can inactivate new toxin not yet bound. Toxin that is already bound to nerves simply has to unbind in time on its own. There is a risk in using antitoxin because it is a blood product of another species and highly inflammatory to the immune system. Antitoxin can be given under the skin or in the muscle but can take up to 3 days to reach a therapeutic level this way. Giving it by IV is more rapid but also more dangerous in terms of inducing an anaphylactic reaction. Skin testing is commonly used to see how reactive the patient might be. It is potentially helpful in early stages of disease only.
Tetanus toxoid is the tetanus shot most of us have had at one time or another. It is a vaccine against the tetanus toxin and it is part of a horse’s regular vaccination set, just as it is part of a human’s vaccination set. Because dogs and cats are much more resistant to tetanus than horses and humans, regular vaccination against tetanus is not recommended for them.
Nursing care requires a darkened room with minimal stimulation even if the pet no longer requires hospitalization. Clenched jaws can be problematic for feeding so expect a liquid diet or slurry to be needed. Soft bedding to prevent bedsores is a must.
Improvement is generally noted within the first week of therapy but complete recovery can easily take a month.
Some Tetanus Statistics
Most of the information in this article has been gleaned from a study by Burkitt et al published in the Journal of the American Veterinary Medical Association in January 2007 where 35 cases of canine tetanus seen at the University of California Veterinary Teaching hospital were reviewed for analysis.
Severity Classes
For the purposes of the study mentioned above, cases were classified by the severity of their signs into four groups. It is important to realize that a dog’s initial classification could easily change (in this study 17 dogs that were normal or in Group I at the beginning of the study ended in Group III or IV).
|
Group I
|
The dog was able to walk but also demonstrated constricted pupils, risus sardonicus, erect ears, inability to open its jaws, sunken eyes, and/or sensitivity to light.
|
|
Group II
|
All of the above plus erect tail, sawhorse stance, difficulty swallowing, walking stiffly with difficulty.
|
|
Group III
|
All of the above plus muscle tremors or spasms, inability to walk, and seizures.
|
|
Group IV
|
All of the above plus any of the following: heart rate below 60 beats per minute, heart rate above 140 beats per minute, high blood pressure, low blood pressure, or respiratory arrest.
|
Foxtail

Photo courtesy of Dr. Wendy Brooks
Overall, of the 35 dogs included in the UC Davis study, 77 percent survived. All of the dogs that did not progress beyond the severity of Group II survived and 50% of the dogs in Groups III and IV survived. Dogs in these latter two groups required continuous care (intravenous fluids, sedation, nutritional support, etc.)
In 27 percent of cases, the initial wound was a foxtail tract and an additional 50 percent of wounds were suspicious of foxtail tract. A foxtail, or grass awn, is a sharp plant tuft that easily gets caught in fur and migrates deep into a wound, ending up in an assortment of inopportune areas of the body. An important conclusion of this study was that the wound need not be a bite or traumatic puncture.
Recovery of an Extreme Case
This video shows an extreme case of tentanus. University of Florida veterinarians saved the dog.