VP_raccoon_shutterstock_133885685.jpg

Raccoon
Descriptions of rabies go back thousands of years, as rabies has classically been one of the most feared infections of all time.
It is because of rabies that dog ownership virtually everywhere in the U.S. requires a license and documentation of rabies vaccination. There is still no reliably effective treatment for rabies infection once symptoms have started. In other words, if you get rabies and it progresses to showing symptoms, you will almost certainly die within days, and even in the 21st century, this remains true. The virus does not survive very long outside of the infected host, so transmission requires direct contact with fresh secretions. In most cases, this means a bite wound, and it usually involves wildlife infecting other wildlife with no humans or pets involved.
When wildlife starts coming into contact with the pet population, pets become infected, and when pets get infected, human infection is not far behind. Because this infection has nearly 100% mortality, preventing it in pets becomes crucial to preventing it in people. Of course, people can get infected by wildlife contact as well. Despite vaccination being readily available, every year, the U.S. reports approximately 50 canine deaths, 250 feline deaths, and several human deaths from rabies. Worldwide, some 55,000 human deaths occur annually from rabies in the 21st century.
The most common wildlife species to spread rabies to domestic animals and humans in the Northern Hemisphere are skunks, bats, raccoons, foxes, and coyotes. Wildlife (especially bats) can gain access to indoor areas where they can come in close contact with both pets and people. Indoor pets are not without risk.
Many people do not realize how fast death occurs from rabies.
VP_redfox_shutterstock_1682308579.jpg

Red fox
While it may take a long time for the virus to incubate, once even mild symptoms begin, death occurs within 10 days.
The injection treatment most people have heard of only works during the incubation period; once symptoms have started, survival chances are slim.
The Course of the Disease
The virus in the infected animal's saliva enters the victim's tissues during the bite. The virus attaches to the local muscle cells for a couple of days before penetrating local nerves and beginning its slow ascent to the brain. Once within nervous tissue, the virus is not accessible to the immune system and may safely proceed toward the brain. The journey is slow and can take up to a year, but the average time is three to eight weeks, depending on the species. After the virus enters the brain, it only takes two to three more days for it to become evident in all body secretions, including saliva. At this point, all fresh body secretions can transmit the rabies virus, and symptoms begin.
It can take up to a year from the time of the initial bite before symptoms begin to show. In dogs, typical incubation periods are 21-80 days. In cats, it's 28-42 days. Once symptoms show, treatment is nearly impossible.
Prodromal Stage (The First Two to Three Days After Symptoms Have Started)
A personality change is noted. Friendly animals become shy, etc. The larynx begins to spasm, and a voice change may be noted (especially in rabid cattle). Most infected animals will actively lick or scratch the site of the original bite.
Excitative Stage (Next One to Two Days)
Classically, this would be the "mad dog" stage, though most animals skip this phase altogether. The animal has no fear and suffers from hallucinations. If confined, the animal often attacks the cage bars.
Paralytic or Dumb Stage (Next Two to Four Days)
Weakness/paralysis sets in. The larynx is paralyzed, resulting in an inability to swallow, thus drooling and "foaming at the mouth" result. The animal dies when the breathing muscles are paralyzed. It is from animals in this stage where most human exposure occurs. There is no treatment for animals or humans once clinical signs appear.
VP-skunk_AdobeStock_181031715.jpeg

Skunk
Once the virus has been released to body secretions, it is again accessible to the immune system; however, the patient dies before an adequate immune response is mounted.
The classical symptoms of rabies described above may not be recognizable, making diagnosis difficult, if not impossible, in a living animal. Long quarantines are often needed to determine if the infection has occurred.
When human exposure to the animal in question is involved, what happens depends on several criteria. If the animal in question is dead, its brain can be tested for rabies. There is no test for rabies in a living animal, but since it is known that death follows quickly after the virus becomes contagious, a living animal can be confined for 10 days. If the animal is still alive 10 days after biting a person, then the bite could not have transmitted rabies.
Prevention
For Your Pets
Happily, rabies prevention is accomplished with vaccination and limiting exposure to wildlife. The standard killed virus vaccines are available for both dogs and cats, and after the initial dose, which is good for one year, subsequent doses are generally good for three years. Because tumors have developed in cats who received the killed virus vaccine, a recombinant product is now available that uses a portion of rabies viral DNA cloned into a harmless canarypox virus. This arrangement allows the pet to realize the benefits of live virus vaccination without any risk of exposure to the living rabies virus.
Rabies vaccination protocols are typically controlled by municipal regulations. Most communities legally require the vaccination of all dogs. The American Association of Feline Practitioners recommends rabies vaccination as a core vaccine for all pet cats.
For pets not current on rabies vaccination that have been exposed to biting wildlife, the Texas Post-Exposure Rabies Prophylaxis Protocol has been particularly helpful. In this situation, the pet should be vaccinated for rabies as soon as possible after the wildlife bite, and booster vaccines should be given three weeks post-bite and eight weeks post-bite. The pet should be strictly isolated for 90 days. This protocol has been extremely successful in preventing rabies symptoms and contagion when normal rabies vaccination has lapsed.
VP_coyote.jpg - Caption. [Optional]
![VP_coyote.jpg - Caption. [Optional] Coyote standing in woods](/AppUtil/Image/handler.ashx?imgid=7497535&w=175&h=271)
Coyote
Treatment for Humans (Post Exposure Prophylaxis or PEP)
As mentioned, once symptoms have started, treatment can be attempted, but truly, there is little chance of survival. The only way to survive rabies is to exploit the long incubation period and basically get vaccinated quickly. Doing this involves a very big piece of information: knowing you were (or may have been) exposed. Every year, a small number of people die of rabies in the U.S. Most of these people were bitten by a dog, bat, or some other animal and did nothing other than basic first aid. Recall that it takes many weeks for the rabies virus to reach the brain. This allows time for the vaccine to be given so that when the virus "comes out" of its neurologic hiding place and is ready to infect the brain, a substantial immunologic response is waiting. The virus is foiled, and clinical rabies does not result.
If you are bitten by an animal and its rabies vaccination history is unknown, there are definite steps to take. A fresh bite wound should be washed out with water quickly, as this may wash out viral particles. The time it takes for the virus to reach the brain depends on the amount of the virus and how close the wound is to the head. This simple step can be life-saving.
If the biting animal is alive, its vaccination status should be confirmed as soon as possible, and it will need to be confined according to local law. The bite wound should be reported to the health department as soon as possible. Only rodent and rabbit bites are not reportable.
If the animal is dead, its brain can be tested for rabies. The head of the biting animal is submitted to the health department for fluorescent antibody testing for the rabies virus. This process takes a matter of hours, so any bite victims can know right away if they will require rabies treatment.
If the animal is not available or its vaccination status is in question, further treatment may be needed. Hyperimmune (antibody-rich) serum is flushed into the wound in the hope of inactivating the virus before it penetrates the nerves. The patient receives a vaccination on a regular schedule for about a month, as described above.
Veterinarians have a rabies exposure risk of more than 300 times that of the general population.
Anyone pursuing a career with animals should consider vaccination against rabies.
VP_Rabies Virus_AdobeStock_221349693.jpg
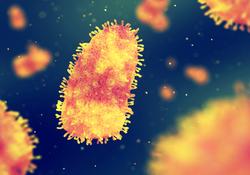
Rabies virus
The Law Regarding Animal Bites (Against Humans)
In the U.S., states and counties have different regulations regarding rabies vaccines for companion animals and bites to humans. Regulations for your area in the U.S. can be found through your county's health department. In almost all states in the U.S., the biting animal must be confined for observation for 10 days at the owner's expense, regardless of vaccination status.
The quarantine period is to determine whether the rabies virus was present in the animal's saliva at the time of the bite.
An animal infected with rabies and shedding virus will certainly be dead within ten days. One might want to know why quarantine is still necessary if the animal is vaccinated, and the answer has to do with the seriousness of a rabies infection. No vaccine is 100% effective, so it is important to be certain in order to prevent human exposure.
The situation is different if the biting animal is known to have been exposed to wildlife. A vaccinated animal must be re-vaccinated within the time period required by local regulations and confined for observation for the specified duration. Unvaccinated animals may be confined for a specified time period according to local/regional law or be euthanized and tested for rabies. In the U.S., all bites to humans that break the skin are reportable to local health departments. Rabies vaccination requirements vary from state to state and county to county. Contact your veterinarian if you think your pet has come into contact with or been bitten by a wild animal. Regardless of the vaccination status of your pet, wild animal bites may lead to painful wounds and infection.
Again, laws regarding biting dogs and rabies vaccination are highly regional. Check with your local animal regulation department, your veterinarian, or visit rabiesaware.org to find out what you need to know in the U.S..
Quarantines when Traveling
Great Britain, Hawaii, Japan, New Zealand, and several other island areas have successfully eradicated rabies from their territory. These places are EXTREMELY cautious about allowing in potential carriers of rabies. A very long quarantine is needed because of the long incubation period of rabies; however, this must be balanced by the expense associated with quarantine and owners' reluctance to be separated from their pets. Most places that have eradicated rabies have protocols for avoiding or minimizing quarantine. Typically, a microchip is implanted in the pet for identification purposes, a rabies antibody titer (a measurement of vaccine-induced protection) must be performed at an approved laboratory, and rabies vaccine documentation is necessary.
For listings of what each state requires for entry, go to the USDA.
For travel to another country, check with that country's consulate, but guidelines are also available at USDA.
Other Links
The CDC's rabies home page has basic information and a children's education area that is particularly helpful for families who go camping.
The annual World Rabies Day calls attention to this problem to raise awareness and provide information about rabies in both humans and animals.
In Summary:
You can’t treat rabies once symptoms set in; all you can do is prevent it.
Rabies is a virus transmitted through saliva or brain tissue. Without rapid preventive treatment, it is almost always fatal. That’s why your pets are required to have rabies vaccines in many areas of the world.
The most common wildlife species to spread rabies to animals and people in the Northern Hemisphere are bats, skunks, raccoons, foxes, and coyotes.
It is generally caused by a bite wound, and wildlife is mostly infected.
Rabies affects a mammal’s central nervous system. It can take up to a year before symptoms begin to show, but the average time is three to eight weeks depending on the species. In dogs, the typical incubation period is 21-80 days. In cats, it's 28-42 days. Once symptoms begin, treatment is nearly impossible.
If you are bitten, you need a preventive injection immediately, as it only works during the incubation period. Once even mild symptoms begin, death occurs within 10 days.
After symptoms have started:
- First two to three days: a personality change is seen, and the larynx spasms, resulting in a voice change.
- Next one to seven days: this is the “mad dog” stage in which an animal has no fear and suffers from hallucinations, but many skip this stage.
- Next two to four days: weakness and paralysis set in. The larynx becomes paralyzed so the animal cannot swallow, causing drooling and foaming at the mouth.
- The animal dies when the muscles that control breathing finally become completely paralyzed. Most people get bitten in this stage.
Symptoms may not be obviously recognizable, making diagnosis difficult if not impossible. As of the time of this writing, there is no diagnostic test for rabies in a living animal.
What happens after people are exposed depends on the situation. If the animal is dead, its head is sent to a laboratory so the brain tissue can be tested. In some circumstances/locations, a living animal can be quarantined for 10 days at the owner’s expense; if the animal is still alive, then the bite could not have transmitted rabies.
The vaccine protocols are typically controlled by municipal regulations. Most communities legally require all dogs to be vaccinated and recommend it for cats. Vaccination requirements vary from state to state, and county to county.
Exposed pets not current on rabies vaccination should be given booster vaccines at three and eight weeks post-bite. The pet should be strictly isolated for 90 days.
Exposed humans should wash the bite with water as it may wash out some virus particles; the time it takes for the virus to reach the brain depends on the amount of virus in addition to how close the wound is to the head. This step could save a life.
Animal bites need to be reported to local health departments.
Veterinarians have a rabies exposure risk of more than 300 times that of the general population. Anyone in an animal-oriented job should consider preventive vaccination. Back to top