Abstract
Since 1995, at least three anesthetized polar bears have died while suspended in nets during research and management programs. A study was undertaken to determine the effect of suspension by net on the cardiopulmonary function of anesthetized polar bears. Eight captive polar bears were anesthetized with Telazol® (mean=9.5 mg/kg, SD=2.29 mg/kg). Arterial blood pressures of anesthetized polar bears increased significantly, and failed to return to baseline values, when the bears were suspended in the net. Bears are at risk of developing clinically significant acute hypertension following net restraint. It is recommended that alternative methods of suspending anesthetized bears above the ground for purposes of research and management be considered.
Introduction
In the management, conservation, and research of captive and free-ranging wild species, anesthetized animals are often restrained and positioned in different postures, some of which may markedly compromise cardiopulmonary function. However, the cardiopulmonary effects of restraint and posture have received little attention in wildlife anesthesia, although they are well-documented in human and domestic animal anesthesia.8-11 In our ongoing investigation of the physiology of polar bears (Ursus maritimus), we often restrain and suspend anesthetized polar bears by net for up to 5 minutes to enable us to determine their body mass. Similarly, during wildlife management operations, anesthetized polar bears are translocated while suspended in a cargo net beneath a helicopter for flights lasting between 20–30 minutes. Since 1995, at least three anesthetized polar bears have died while suspended in nets during research and management programs but, in all cases, the cause of death remains unknown.2,3 In an effort to improve methods of anesthetizing and handling polar bears, and to potentially reduce anesthesia-related morbidity and mortality in these animals, we designed and conducted a study to determine the effect of restraint and suspension by net on the cardiopulmonary function of anesthetized polar bears. Eight captive polar bears were anesthetized with Telazol® (mean=9.5 mg/kg, SD=2.29 mg/kg).
Materials and Methods
In Hudson Bay, most polar bears naturally fast on land between July and November. During this time, the bay is free of ice and polar bears are no longer able to capture their principal prey, ringed seals (Phoca hispida). However, as the ice begins to re-form in late October, polar bears become increasingly active and begin to concentrate along the Hudson Bay coast, and in the vicinity of Churchill. Those bears posing a threat to the inhabitants of Churchill are captured by the Manitoba Department of Natural Resources and moved to a restricted-access facility within which they are maintained in individual pens. Once the ice re-forms over Hudson Bay, captive bears are anesthetized and translocated from Churchill to the coastal sea-ice by helicopter.
Eight captive polar bears were anesthetized with Telazol® (mean=9.5 mg/kg, SD=2.29 mg/kg) by pole syringe during November 1997, at Churchill, MB, Canada. Anesthetized polar bears were prepared for cardiopulmonary measurements by aseptically cannulating their femoral artery with an 18-g × 10-cm arterial catheter. The catheter was subsequently secured with ligatures and connected to a pressure transducer, via non-compliant plastic tubing filled with heparinized saline. The transducer was calibrated and connected, in turn, to a physiologic monitor used to measure direct systolic, mean, and diastolic arterial pressure, and heart rate. Percent saturation of hemoglobin with oxygen (SaO2) was monitored using a reflectance probe inserted in the rectum and connected to a pulse oximeter.
Physiologic parameters measured were arterial pressures, heart rate, respiratory rate, SaO2, and rectal temperature. We collected arterial blood samples at predetermined times for hematology and blood gas analyses. Blood samples were chilled in ice water immediately following collection. Within 3 hours of collection, hematologic, and blood gas analyses were completed using an automated blood counter and blood gas analyzer. All blood gas analyses were corrected for body temperature and hemoglobin concentration.
Complete physiologic measurements were recorded every 5 minutes during three experimental phases. Phases 1 and 3 each lasted 10 minutes, whereas phase 2 lasted 15 minutes. Within each phase, arterial blood samples were collected only during the first and last sets of measurements. During phases 1 and 3, anesthetized polar bears were unrestrained and positioned on the ground in dorsal recumbency. During phase 2, polar bears were suspended in a net from a 3-m high tripod constructed of telescoping aluminum poles. While in the net, bears maintained a semi-seated or reclined position with their head unsupported and either laying forward on their chest or laterally against their shoulder, similar to the posture assumed by bears during helicopter translocations. After measurements were completed, monitoring equipment was disconnected, and the arterial catheter was removed from the polar bear. To statistically compare cardiopulmonary responses among the three phases, we used one-way ANOVA for repeated measures, and the Bonferroni-multiple comparison test.12 Significance was determined for statistical test values where the probability of a type I error was less than 5 percent.
Results
Although no bear appeared at risk of cardiopulmonary failure while suspended in a net, many indicators of their cardiopulmonary function changed significantly among phases. In particular, arterial pressures were significantly greater during phase 2, than during phases 1 and 3 (Figure 1). Anesthetized bears also consistently showed signs of increased arousal (e.g., head, tongue, and limb movement) while suspended in the net. Most blood gas parameters also changed significantly among phases (Figure 1). Arterial blood pH, PaO2, and SaO2 were significantly increased, and PaCO2 was significantly decreased, during phase 3 when compared to values observed during the previous two phases. Arterial base excess and HCO3- concentration did not change significantly among phases.
Figure 1. Effect of restraint and suspension by net on arterial pressure and blood gases of eight anesthetized polar bears
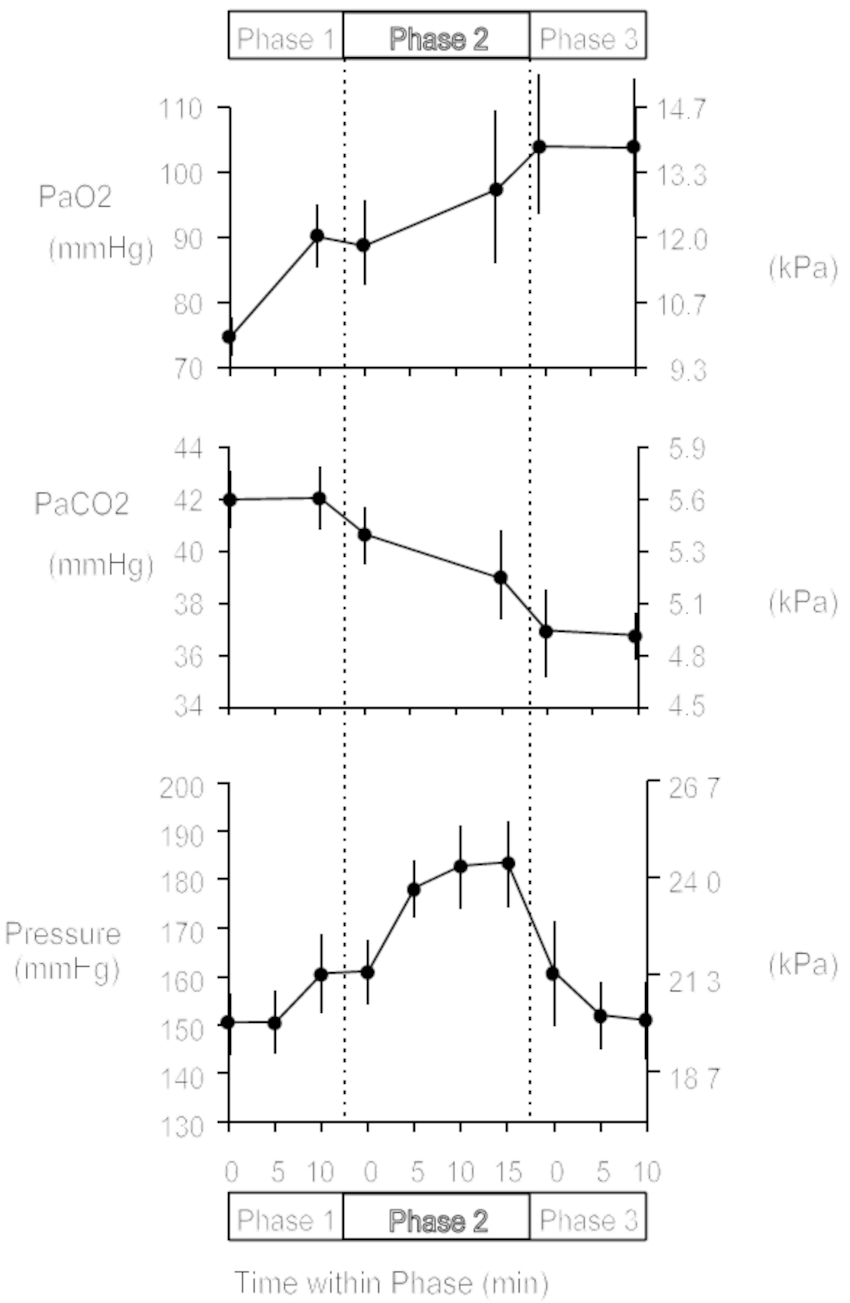
Mean and standard error represented at each measurement time.
Discussion
Arterial pressures typically remain stable during postural changes in awake animals and stabilize to normal values slowly following postural changes in anesthetized animals.9-11 The arterial blood pressures of anesthetized polar bears in this study increased significantly, and failed to return to baseline values, when the bears were suspended in the net (e.g., end-expiration mean arterial pressure increased 17–49% among individual bears). We suggest that the restraint and concurrent body compression imposed during suspension was sufficient to squeeze blood from skeletal muscle and venous reservoirs of the abdomen toward the heart, thereby, increasing venous return. In effect, and possibly mechanism, restraint by net was similar to military anti-shock trousers, an inflatable garment used to combat shock and increase peripheral vascular resistance.5,7 Whatever the mechanism, the acute pressure changes we observed suggest anesthetized polar bears may be at risk of developing clinically significant hypertension when suspended in a net. Arterial pressure did not decrease towards baseline values during the period of suspension, suggesting that additional or alternative mechanisms may have come into effect. One possible explanation is that suspension by net incited a stress response. The resulting sympathetic activity then caused blood pressure to rise by direct cardiovascular stimulation, and by indirect stimulation through the release of epinephrine and norepinephrine into the blood.6 Evidence for a stress response is circumstantial, as we did not measure plasma catecholamine levels. However, we did observe increased arousal of bears suspended in the net, consistent with increased sympathetic stimulation.
Changes in the blood gas parameters of anesthetized polar bears were largely caused by anesthesia with Telazol®, and less so by restraint and suspension by net. The pattern of change in pH, PaO2, PaCO2, and arterial base excess in this study is similar to that observed in previous studies.4 Commonly, pH and PaO2 values progressively increase, and PaCO2 values progressively decrease, following anesthesia with Telazol® (e.g., ≥15 minutes post administration). However, arterial base excess remains relatively static throughout anesthesia such that the combined blood gas results indicate an initial, transient, mild respiratory acidosis. Less apparent, but also common between this study and previous studies, is large variation in blood gas values between individual bears. For example, in this study, when comparing PaO2 values of the arterial blood samples collected from each bear while suspended in the net, the values ranged from 55–137 mm Hg (7.3–18.3 kPa). When examined individually, rather than as the mean, PaO2 value for eight bears, the blood gas responses of some bears indicated they were at risk of developing clinically significant hypoxemia following restraint and suspension by net (e.g., PaO2 ≤60 mm Hg [8.0 kPa] for 3 out of 16 arterial samples collected).
In conclusion, our results indicate that most bears will be at risk of developing clinically significant acute hypertension following restraint and suspension by net as imposed in this study, whereas a smaller number of bears may be at risk of developing serious hypoxemia. We, therefore, recommend developing alternative methods of suspending anesthetized bears above the ground for purposes of research and management. It appears methods using minimal restraint may ultimately prove safer for bears, but this will not be established until newer methods are rigorously compared against existing methods. Finally, we suggest similar studies of cardiopulmonary response to restraint and postural change, in other captive and free-ranging wild species, may contribute to reducing anesthesia-related morbidity and mortality in wildlife research, management, and conservation.
Acknowledgments
We gratefully acknowledge N. Campbell, C. Cassidy, M. Dyck, C. Hutchins, and C. Morran for their assistance in collecting data and analyzing blood samples. We thank the Churchill employees of the Manitoba Department of Natural Resources, particularly Wade Roberts and Jack Batstone, for their cooperation and assistance. This research was funded, in part, by operating grants from the Wildlife Health Fund of the Western College of Veterinary Medicine, the Manitoba Department of Natural Resources Research Fund, the U.S. National Science Foundation, and the National Science and Engineering Research Council of Canada. Further financial and logistic support was received from the Churchill Northern Studies Centre (1997 Northern Research Fund), the Churchill Regional Health Authority, the Medical Research Council of Canada, and the Keewatin Region Health Centre Laboratory.
Literature Cited
1. Anderton, J.M. 1995. Trauma associated with patient transfer and the positioning process. In: T.E.J. Healy, and P.J. Cohen (eds). Wylie and Churchill-Davidson’s A Practice of Anaesthesia, 6th ed., Edward Arnold, London, U.K. 968–992.
2. Calvert, W. 1995. Minutes from the Polar Bear Technical Committee Meeting. Edmonton, AB, Canada. January 31–February 1, 1995. 64 (unpublished report).
3. Calvert, W. 1996. Minutes from the Polar Bear Technical Committee Meeting. Quebec City, QC, Canada. January 31–February 2, 1996. 57 (unpublished report).
4. Caulkett, N.A., M.R.L. Cattet, and S.C. Polischuk. 1996. Comparative cardiopulmonary effects of medetomidine-ketamine and Telazol® in polar bears (Ursus maritimus). In: Proceedings of the AAZV Annual Meeting. Puerto Vallarta, Mexico. 394–400.
5. Gaffney, F.A., E.R. Thal, W.F. Taylor, B.C. Bastian, J.A. Weigelt, J.M. Atkins, and C.G. Blomqvist. 1981. Hemodynamic effects of medical anti-shock trousers (MAST garment). J Trauma. 21:931–937.
6. Guyton, A.C. 1986. Textbook of Medical Physiology, 7th ed. WB Saunders, Philadelphia, PA. 1057.
7. Lee, H.R., W.F. Blank, W.H. Massion, P. Downs, and R.J. Wilder. 1983. Venous return in hemorrhagic shock after application of military anti-shock trousers. Am J Emerg Med. 1:7–11.
8. Rehder, K., and H.M. Marsh. 1984. Gravity, posture, and cardiopulmonary function. In: Mayo Clinic Proc. 59:280–281.
9. Steffey, E.P., A.B. Kelly, D.S. Hodgson, J.L. Grandy, M.J. Woliner, and N. Willits. 1990. Effect of body posture on cardiopulmonary function in horses during five hours of constant-dose halothane anesthesia. Am J Vet Res. 51:11–16.
10. Tagawa, M., S. Okano, T. Sako, H. Orima, and E.P. Steffey. 1994. Effect of change in body position on cardiopulmonary function and plasma cortisol in cattle. J Vet Med Sci. 56:131–134.
11. Wagner, A.E., W.W. Muir, and B.J. Grospitch. 1990. Cardiopulmonary effects of position in conscious cattle. Am J Vet Res. 51:7–10.
12. Zar, J.H. 1996. Biostatistical Analysis, 3rd ed. Prentice Hall, Upper Saddle River, NJ. 662.