State-of-the-Art Lecture Management of Preclinical Heart Disease in Dogs – The EPIC Trial
The results of the EPIC study were published in 2016. The full report of the clinical trial is available as an open access publication at the following link http://onlinelibrary.wiley.com/doi/10.1111/jvim.14586/full
In brief summary – the aim of the trial was to evaluate whether or not dogs with enlarged hearts, secondary to myxomatous mitral valve disease (DMVD), that had not yet developed signs of congestive heart failure, would benefit from the administration of pimobendan.
We tested our hypothesis by conducting a double-blind placebo-controlled trial in which 360 dogs were randomly allocated to one of two treatment groups: pimobendan or placebo.
The primary endpoint of the study was a composite of the onset of signs of congestive heart failure or cardiac-related death (which ever occurred first).
The study demonstrated a clear benefit associated with the administration of pimobendan. The likelihood of a dog reaching the primary endpoint was reduced by approximately one third if it received pimobendan.
The median time to the primary endpoint was approximately 15 months longer in the treated group indicating, on average, a prolongation of the time to the development of clinical signs by over a year.
| Figure 1. A Kaplan Meier survival plot illustrating the estimated time to the primary endpoint in the two treatment groups in the EPIC trial | 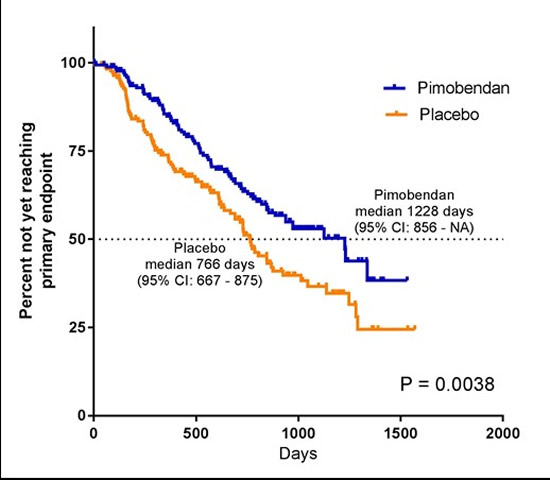
|
|
| |
Ramifications of the EPIC Trial
As a result of the findings of the EPIC study we can conclude that there is a benefit of administration of pimobendan before the onset of signs of CHF in dogs with DMVD. We cannot however conclude that all dogs with DMVD will benefit. No dogs without cardiac enlargement (stage B1 dogs) were recruited to the study and therefore we can only conclude that there is a benefit associated with the administration of pimobendan to dogs with DMVD that have enlarged hearts (i.e., stage B2 dogs).
The majority of dogs recruited to the study were completely free of any outward signs of disease. The majority of the dogs’ owners did not consider their dog to be coughing, nor did they feel that their dog’s exercise tolerance was in any way compromised. This has the important implication that dogs appear to benefit from therapy before they are showing any signs. This in turn means that taking the approach of waiting until signs develop may now result in some dogs being denied potentially life-prolonging and life-improving therapy.
It is this point which highlights the key change in the management of patients with mitral valve disease, which the EPIC study has brought about. Previously, taking a “watch and wait” approach was entirely justified on the basis of the available evidence. A patient would be expected to demonstrate some signs – such as coughing, exercise intolerance or increased respiratory rate – either prior to, or at, the time when the introduction of therapy was justified on the basis of the best evidence available. Now, if one waits until clinical signs are present before investigating a patient’s disease, it is possible that a stage of disease during which that patient would have benefitted from therapy would already have elapsed by the time treatment is started. The opportunity to help that patient would have been missed.
Watching and waiting, although a previously sensible approach, is no longer enough to enable you to offer the best evidence-based care to your patients with DMVD. If you are suspicious that a patient may have progressive DMVD, even in the absence of any outward clinical signs, it is worth investigating further. If such a dog is shown to have cardiomegaly, initiating treatment with pimobendan at that stage will probably result in the dog having a longer period before the development of signs of heart failure and prolong the dog’s life.
How Can Dogs That Will Benefit From Early Therapy Be Found?
It is relevant to ask “how can dogs that will benefit from therapy be identified in practice?” The simple answer is “dogs like those recruited to the EPIC study will benefit from therapy” – therefore, to determine whether or not a dog may benefit from therapy requires one first to be cognisant of the inclusion (and exclusion) criteria of the study. The most relevant ones are reproduced in the table below.
|
EPIC study
|
|
Inclusion criteria
|
• Systolic murmur with maximal intensity over the mitral area (≥grade 3/6)
• Characteristic valvular lesions of the mitral valve and apparatus
• Presence of MR on the colour Doppler echocardiogram
• Echocardiographic evidence of left atrial dilatation 2D LA/Ao ratio ≥1.6 (by the Swedish method)
• LVIDDN≥1.7 according to the Cornell formula
• Radiographic evidence of cardiomegaly VHS score >10.5
|
|
Exclusion criteria
|
• Clinically significant supraventricular and/or ventricular tachyarrhythmias
• Cardiac disease other than MMVD
• Evidence of clinically relevant pulmonary hypertension (RA:RV gradient >65 mm Hg)
|
When results of a clinical trial are generalised to a larger population of dogs, we are assuming that because the drug was shown to be effective in dogs defined by the inclusion criteria of the study – it will be similarly effective in other dogs that share those characteristics. We do not know whether the drug will be effective in dogs that differ from those recruited to the study and therefore we should probably refrain from administering it!
How Are Dogs with Preclinical Mitral Valve Likely To Be Discovered?
A cardinal sign of MVD is the presence of a left apical systolic murmur in a dog of an appropriate age and breed. The murmur is reliably detected on clinical examination (if dogs are auscultated carefully!) and is usually present for years before clinical signs develop.
All dogs recruited to the EPIC study had murmurs that were at least a grade III/VI in audibility (i.e., at least as loud as the underlying heart sounds S1 and S2. If a dog is carefully auscultated and does not have a heart murmur, or has one of a low intensity, it is unlikely to be a dog that will benefit from therapy. A murmur is usually present in dogs with MVD for years before clinical signs develop. In its early stages MVD is usually slowly progressive. For these two reasons, annual auscultation of at-risk dogs will probably be sufficient to identify the presence of disease well before treatment is likely to be necessary. Only dogs with louder murmurs need undergo further investigation (provided it seems clinically likely that the cause of the dog’s murmur is MVD). Dogs with quiet murmurs as a consequence of MVD are very unlikely to have advanced disease. A large majority of the dogs recruited to the EPIC study were considered by their owners to be normal and have no signs attributable to their heart disease. Therefore it is not advisable to wait for signs to develop before considering the introduction of therapy. Dogs with more advanced MVD may be more likely to have higher heart rates and a regular heart rhythm (i.e., have lost the natural variation in heart rate associated with respiration) on auscultation.
Dogs suspected of having more advanced preclinical MVD should undergo diagnostic imaging to determine whether or not its heart is enlarged. Dogs entering the EPIC study underwent both echocardiography and radiography. Of those two techniques, echocardiography is the better test for demonstrating evidence of subtle cardiac enlargement. Ideally therefore, dogs suspected of having DMVD should undergo echocardiography to determine their heart size. This is not to imply that radiography is of no value in determination of heart size. It is very likely that a dog with a clearly enlarged cardiac silhouette on a thoracic radiograph will probably have echocardiographic evidence of enlargement. However, breed differences in heart size (and VHS) mean that where fine distinctions need to be made between normal and enlarged hearts echocardiography is superior.
The echocardiographic criteria used to recruit dogs to the study were relatively simple and therefore a competent echocardiographer should be able to determine whether a dog has evidence of left-sided cardiac enlargement on the basis of two-dimensional and M-mode echocardiographic images obtained from the right parasternal viewing locations.
It is natural to ask whether in order to initiate pimobendan therapy in a dog with preclinical MVD the dog must first undergo echocardiography. Where a dog has considerable cardiomegaly evident on radiography, it is probably safe to assume there will also be cardiomegaly evident on echocardiography. The cut-off of 10.5 for vertebral heart score used in the EPIC study is too lenient to use as a sole criterion for initiating therapy because a number of normal dogs of certain breeds will exceed this value. A group of cardiologists in the US – the “Cardiac education group” – have prepared a useful algorithm.1 They recommend that where access to echocardiography is limited, a VHS of 11.5 or a rapid rate of increase of VHS may be used as a way to identify dogs that may benefit from therapy. It is however worthy of note that more than half the dogs enrolled in the EPIC study had a VHS lower than 11.5; meaning that applying this criterion alone would result in many dogs that may benefit from therapy not receiving it.
Whether there are other methods by which dogs that will benefit from therapy can be reliably identified is currently not known and therefore initiating treatment in the absence of diagnostic imaging is not recommended.
Resources
1. http://cardiaceducationgroup.org/wp-content/uploads/2016/12/CEG_Recommendations_EPIC_121316.pdf