Top Tips in How to Reduce and Align Fractures: Minimal Effort for Maximum Outcome
Reduction is the process of either reconstructing the fractured bone to its normal anatomy by restoring the correct position of the fragments or restoring the normal alignment of the limb.
Conceptually, reduction of a fracture reverses the process which created the fracture displacement during the injury and needs the application of forces and movements opposite to those that produced the fracture.
Consequently an accurate analysis of the level of displacement and degree of deformation represents a fundamental help in planning the strategies needed to achieve reduction.
These concepts apply despite the reduction method applied, be it open or closed, manual or by skeletal traction, with or without instruments.
When a bone is fractured, the continuous tension generated by the muscle contraction, provokes shortening and overriding of the bone ends. The initial muscle spasm is aggravated by the concomitant injury of the soft tissues of the affected area. Post-fracture oedema and haematoma will form within a few hours post injury and will fill the interstitial spaces and create fluid-filled voids along tissue planes around the fractured area. The oedema generates hydrostatic forces that create additional shortening of the fractured extremity and an additional impediment to fracture reduction. After several days, the inflammatory reaction in the area accompanied by proliferating changes leads to contraction of more permanent nature, making the reduction attempts even more difficult.
Objectives of Fracture Reduction
In diaphyseal and metaphyseal fractures, the aim is to restore as precisely as possible the length, the axial and rotational alignments of the bone. Axial bending in the sagittal plane is usually well tolerated unless it is generating excessive limb shortening. A moderate degree of varus angulation of the distal segment is generally better tolerated than valgus angulation that usually leads to significant functional problems.
Articular fractures demand anatomical reduction and absolute stability to enhance the healing of the articular cartilage and make early motion possible.
Residual displacement should not be tolerated in order to avoid the development of post-traumatic osteoarthrosis. Unfortunately, this is not always possible, and a better reduction cannot be achieved without additional soft tissue damage, an extended or combined surgical approach, with consequently increased surgical time—all this increasing the risk factors and morbidity.
In these cases, we have to consider that “better is enemy of good” and a less perfect reduction can be acceptable for the sake of respecting the local biology.
The secret of reduction is the application of continual steady traction over time. This will fatigue the muscles allowing reduction.
Methods of fracture reduction include open or direct reduction and closed or indirect reduction.
Closed Reduction
Reduction is obtained by application of traction, countertraction and manipulation of the limb. The fracture is not directly exposed, and the fracture area remains covered by the surrounding tissues.
This method is ideal provided that it can be accomplished with minimal tissue trauma.
Traction can be applied either manually or by gravity.
To apply manual traction, the patient (under general anaesthesia) is positioned on a table on lateral recumbence on the side opposite the fractured limb. A soft rope loop or a padded belt is placed around the axillary or groin region and is secured to the edge of the table near the patient’s back. A second rope loop is placed in the carpal or tarsal area, and slow, continuous traction is applied. Manual traction is quite demanding and is difficult for the surgeon to be able to apply a slow and progressively increasing traction over the 10 to 30 minutes that are usually necessary to fatigue the muscle. The Gordon’s extender is a mechanical device that allows traction to be exerted without the surgeon exerting as much force.
The animal weight can be used to advantage when using gravity to obtain traction. The patient is placed on dorsal recumbence, and a piece of tape, gauze or soft rope is placed around the metacarpal or metatarsal area of the affected limb. The attaching material is connected to an infusion stand or to a secure bolt in the ceiling and is pulled enough to raise the animal slightly off the table so that part of the bodyweight is producing traction on the suspended limb. Traction can also be modulated by temporary lowering of the table.
When adequate traction is obtained, usually after 10 to 30 minutes, it is possible to reduce the fracture by manipulation of the more movable fragment.
When performing manipulation, always be alert to the possibility of laceration, perforation or compression of neurovascular structures.
Open Reduction
In open reduction, the fracture lines are exposed surgically, and the bone fragments are reduced under direct vision with instruments applied directly to each fragment, usually near the fracture side.
Open reduction is usually indicated for articular fractures, fractures that are unstable and complicated, fractures of several days of duration and those fractures that require internal fixation.
Reduction techniques must be gentle and atraumatic.
A good preoperative planning includes a good knowledge of the anatomy and surgical approach to the area.
The surgeon should make every effort to respect any remaining vascularity and to avoid soft tissue stripping in order to preserve the biologic healing potential. Keep in mind that increased injury trauma requires decreased surgical trauma.
Strict haemostasis should be obtained by conscious use of electrocoagulation. A combination of frequent, copious irrigation with Ringer’s solution and gentle suction helps to maintain a clean area allowing good visualization of the operative field. The fragments are handled carefully during exposure and reduction, in order to preserve any soft tissue attachment.
If anatomical reconstruction is possible, the fragments are fixed in place with lag screws, wires or Kirschner wires. Fragments that are too small for internal fixation should be left untouched to preserve their blood supply.
As a general rule, all fragments must be kept whether or not they have soft tissue attachments, as they will function as an autogenous bone graft.
Instruments and Methods of Open Reduction
Bone Holding Forceps
The fracture can be reduced with application of direct force using bone holding forceps on one or more bone fragments (Figures 1a, 1b).
| Figures 1a (left), 1b (right) | 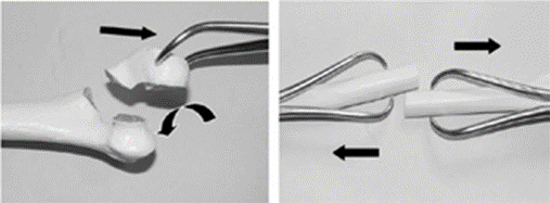
|
|
| |
An oblique fracture overriding can be reduced with a bone holding forceps grasping obliquely each main fragment. With some pressure and simultaneous rotation of the handles, the bone is lengthened and the fragments are reduced (Figures 2a, 2b).
| Figures 2a (left), 2b (right) | 
|
|
| |
The disadvantage of this technique is the tendency of the forceps to slip on the bone surface, adding further damage to the periosteal sleeve.
One other application consists of grasping each of the two main fragments of a transverse fracture with pointed reduction forceps; lengthening is achieved by manual distraction while proper axial alignment can be controlled with the forceps (Figure 3a).
| Figure 3a | 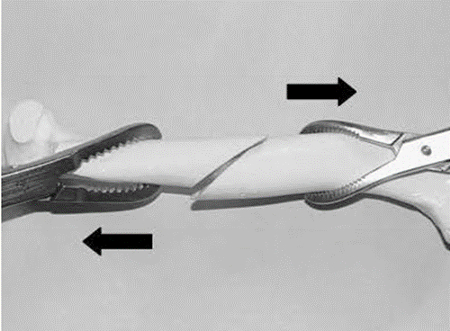
|
|
| |
In an oblique diaphyseal fracture, reduction is secured with the application of another pointed reduction forceps applied more or less perpendicular to the fracture plane (Figure 3b).
| Figure 3b | 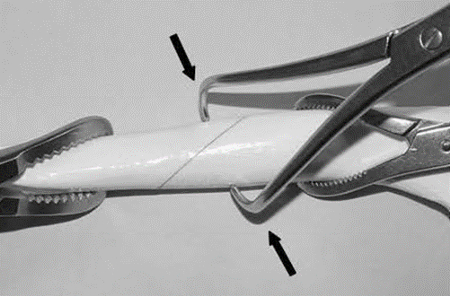
|
|
| |
In a simple transverse fracture, the primary intrinsic stability ensues, allowing removal of the clamps without loss of reduction.
The reduction can be facilitated by the combined levering action of a Hohmann retractor or a periosteal elevator (Figure 3c).
| Figure 3c | 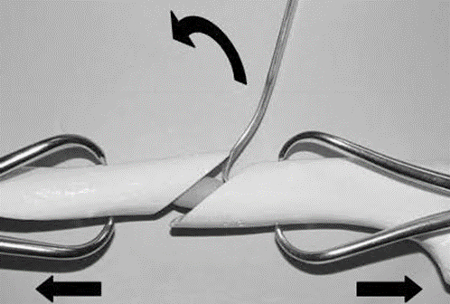
|
|
| |
All reduction maneuvers with use of bone clamps depend on the friction between the bone forceps and the bone being greater than that between the bone fragments.
In order to avoid complications related to the use of bone clamps, few guidelines should be followed:
Some of the clamps (e.g., Lohman clamp) cause extensive periosteal stripping. The pointed reduction forceps (Weber tenaculum) are the least atraumatic, as they are gentler to the periosteal sleeve.
Bone fragments should be carefully inspected for fissure fracture lines; application of pressure in a fissured bone fragment or accidental insertion of the tip of a pointed reduction forceps in a fracture line can increase the level of comminution. Weak bone segments can be supported by application of cerclage wire before attempting reduction. Use bone clamps cautiously in young patients, as it is possible to crush the bone in the attempt of achieving adequate friction between bone and the forceps.
Bone clamps are also useful to correct a residual axial malalignment in the sagittal plane when plating a long bone fracture. After the fracture has been grossly aligned, a plate is applied and secured to one fragment, one tip of the clamp (usually a Verbrugen self-centering clamp) grasps the anterior or posterior aspect of the bone while the other tip engages on the plate’s border. By closing the clamp, it is possible to create a shift of the bone fragments and correct the malalignment.
Special reduction clamps are available to overcome the most difficult situations. The Farabeuf clamp and the pelvic reduction forceps (Jungbluth clamp) are designed to grasp screw heads introduced in both sides of a fracture line. These clamps allow application of compression, limited lateral displacement, and in particular the Jungbluth clamp permits a certain amount of distraction. These clamps are extremely useful for reduction of pelvic fractures.
Hohmann Retractor
A small-tipped Hohmann retractor is an extremely useful instrument that can be used to apply levering or as a pusher to achieve reduction. A classic application of this instrument is in the reduction of simple diaphyseal fractures. The tip of the Hohmann retractor is gently inserted in the fracture gap between the two cortices, is then turned 180 degrees to engage with its tip the cortex of the opposite fragment. Gradual and gentle application of bending force on the retractor allows reduction of the fracture (Figures 4a, 4b).
| Figures 4a (left), 4b (right) | 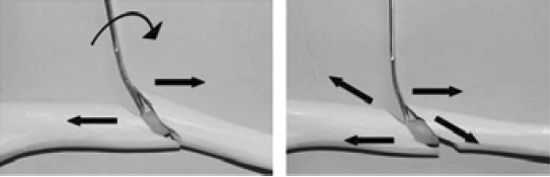
|
|
| |
To correct minimal lateral displacement it is possible to turn the retractor so that the fragments can slide on each other. When reduction is satisfactory, the retractor is removed by turning and bending to decrease the leverage and sliding it out. Another common application of the Hohmann retractor is in the reduction of fractures of the ileum following the same modalities described above. Other instruments such as small osteotome, a periosteal elevator or a scalpel handle can be used to apply leverage in the same fashion of the Hohmann retractor.
Use of Implants for Reduction
Implants can contribute to the reduction as well as stabilization of a fracture. An example of this is reduction obtained with a Steinmann pin used as a fracture distractor. This simple method can be applied to fractures of the humerus, femur and tibia. The pin diameter should be about 50% of the medullary canal and is inserted in a normograde manner. As the nail crosses the fracture line and is driven into the distal fragment, reduction must occur. Cutting the tip of the pin before its insertion into the distal fragment limits penetration of the pin in the metaphyseal bone.
Reduction is facilitated by the use of bone clamps and by gentle hammering of the pin further distally avoiding rotational action. In a reconstructible fracture, once a satisfactory reduction has been achieved, it is possible to secure it with bone clamps, cerclage wire or lag screws and gently withdraw the pin before plate application. In comminuted fractures where the bone column is not reconstructible, the pin is left in place after optimal alignment and length are achieved and a plate is applied in a splinting fashion.
Application of a plate on a straight portion of the diaphysis helps restore alignment while the plate acts as a splint maintaining reduction before definitive fixation.
In a short oblique diaphyseal fracture, it is possible to obtain reduction with the aid of a plate in the following manner. The plate is secured on one main fragment, and an independent screw is inserted on the opposite fragment. By pushing and pulling with a laminar spreader placed between the end of the plate and the screw and with reduction forceps it is possible to distract and reduce the fracture (Figure 5).
| Figure 5 | 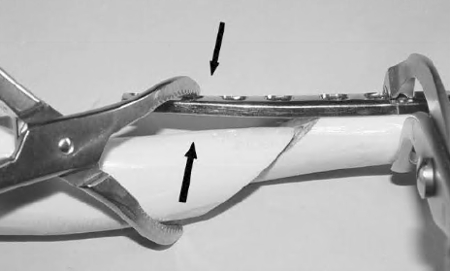
|
|
| |
For ileal body fractures, distal radius and tibia fractures, a plate can be precisely contoured and secured with screws on one bone segment, a bone clamp placed between the plate and the second bone segment allow gradual reduction of the fracture. When the fracture is reduced, the bone clamp is tightened and the plate is fastened with screws.
To correct small displacement and angulation of an oblique metaphyseal fracture, it is possible to use a properly contoured plate in an anti-glide function. The plate is applied to one fragment, and tightening the screws forces the opposite fragment to glide down the oblique fracture plane, obtaining reduction and maintaining stability at the same time.
Joystick Reduction
It is a very simple technique that allows reduction of small fragments in metaphyseal or articular fractures. Insertion of small threaded K-wires allows manipulation of the bone fragments with or without direct view.
Instrumental reduction has its advantages but comes at a price to the fracture biology. The surgeon should keep in mind that “The repeated use of bone clamps and other reduction tools or implants may completely devitalize the fragments in the comminuted area, which may have disastrous consequences for the healing process, including delayed union, non-union, infection or implant failure.”
Fracture Distractor
The fracture distractor (Synthes, Ltd., Paoli, PA, USA; Jorgensen Laboratories, Loveland, CO, USA) is an instrument that allows distraction of the fracture by means of two pins inserted through both cortices in the proximal and distal metaphysis of the fractured bone. After insertion, the fixation pins are attached to the distractor with finger nuts. The distraction is applied by turning the wingnuts on the connecting threaded rod. As there is an inherent tendency of curved bones to straighten during distraction, angular and rotational corrections are usually necessary before definitive fixation. The mechanical advantage of the distractor is that it allows easy distraction of the fragments; but when it is under load alignment, corrections can be difficult. The fracture distractor can be used either in open reduction or closed/indirect reduction.
Indirect Reduction
Increased understanding of fracture healing brought the concept of “biological internal fixation” that represents one of the major conceptual changes of the last decade.
The principle consists of minimizing the biological damage from the surgical approach and the implant contact. This principle is achieved at the expense of less precise reduction and less rigid fixation. The method of absolute stability by compression fixation is supplemented by the method of relative stability by splint fixation that results in a flexible fixation that stimulates callus formation.
The biological internal fixation comes together with the technique of indirect reduction that greatly reduces the surgical trauma and helps to keep bone fragments vital.
In indirect reduction, the fracture lines are not directly exposed, the fractured area remains covered by the surrounding soft tissues. Reduction is accomplished by using instruments or implants that are introduced away from the fractured zone. The technique is indicated for multifragmentary diaphyseal and metaphyseal fractures. The aim of indirect reduction is to restore the overall length of the bone, as well as the axial and rotational alignments.
The technique is more demanding than direct reduction and requires an accurate preoperative assessment and meticulous planning. Reduction is controlled by the help of image intensifier, clinical checks for the alignment or intraoperative x-ray. The techniques for fixation are: interlocking nail, external fixation, splinting with conventional plates, plate and rod, bridging the fracture with a locked internal fixator as the LCP (locking compression plates).
Conclusions
In conclusion, either direct or indirect reduction are useful techniques and have their place in the repertoire of the orthopaedic surgeon. A clear understanding of the role of these techniques, together with an informed assessment of the relationship between fracture pattern and soft tissue trauma, lead to correct decisions on strategies and choice of implants compatible with the biological demand of the fracture.
New principles and methods will continue to develop; however, some principles will never change:
“There is danger inherent in the mechanical efficiency of our modern methods. Lest the craftsman forget that union cannot be imposed but may have to be encouraged for the bone is a plant with its roots in the soft tissues.
“When the vascular connections are damaged, it often requires not the technique of a cabinetmaker but rather the patient care and understanding of a gardener.”
—Dr. Girdlestone (Orthopaedic influence on the treatment of fractures, a clinical study. Oxford 1943)
References
References available from author upon request.