Marc Vandevelde, Prof. Dr.med.vet., DECVN
INTRODUCTION
Canine distemper virus (CDV) is a nonsegmented, single stranded RNA virus and is a member of the Morbilliviruses. The molecular biology, the different CDV strains and their host range have been reviewed in several publications. Despite widespread use of vaccination, distemper continues to be a problem with outbreaks occurring in canine populations but also in other species.
CDV is generally transmitted as an aerosol infection to the upper respiratory tract. The primary virus replication takes place in the lymphoid tissues, leading to severe long lasting immuno-suppression. T cells are more affected than B cells and CD4+ lymphocytes are rapidly depleted for several weeks whereas CD8+ cells are less severely affected and recover relatively fast. At about 10 days p.i., CDV starts to spread from the sites of primary replication to various epithelial tissues and the central nervous system (CNS). As a result of epithelial infection, a variety of respiratory, intestinal and dermatological signs can occur. The most serious complication is infection of the CNS, leading to a variety of neurological syndromes, frequently with bad prognosis.
What can we do against this disease? There are basically 2 avenues of research: 1. Understanding the mechanisms by which CDV causes damage to the nervous system can help to design new therapies. 2. prevention of the disease by designing new and better vaccines.
The brain lesions in nervous distemper
CDV causes multifocal lesions in the gray as well as in the white matter of the CNS. The demyelinating lesions are not only responsible for severe neurological signs but are also thought to be a model for human demyelinating conditions such as Multiple Sclerosis. Therefore, the pathogenesis of demyelination in distemper has been closely investigated. In the following sections, we will focus on what is known about the pathogenesis of the white matter lesions in distemper.
Pathogenetic studies have to consider an acute and a chronic stage in the development of CDV induced demyelination. The initial demyelinating lesions occur around 3 weeks p.i. and evolve during a period of massive virus induced immuno suppression. Depending on the degree and speed of immune recovery, animals may either become quickly moribund or may recover after developing a mild or even subclinical illness. An intermediate group of animals recovers slowly or partially and tends to develop a chronic or even relapsing disease with progression of the demyelinating lesions as a result of immunopathologic reactions.
Acute CDV induced destruction of the white matter
Viral replication in the cells of the white matter
The initial myelin lesions develop during a period of severe immunosuppression and are not inflammatory. Several immunocytochemical studies and recent in situ hybridization work in spontaneous and experimental distemper have clearly shown that demyelination coincides with replication of CDV in the glial cells of the white matter. Spatio-temporal studies leave no doubt that the initial white matter lesions are associated with viral activity and that their development is highly predictable. The obvious explanation for the phenomenon of demyelination would be infection of oligodendrocytes, the myelin producing cells. Therefore, research has focused on finding evidence of CDV in oligodendrocytes. At the light microscopic level, it has been shown that the majority of infected cells are astrocytes. Most electron microscopical studies agree that oligodendroglial infection is very rare in distemper. Only very few oligodendrocytes containing CDV protein were found at the light microscopical level. However, 8% of the oligodendrocytes at the edge of lesions contained CDV mRNA. We found this restricted infection of oligodendrocytes earlier in dog brain cell cultures in which virulent CDV causes a slowly spreading non-cytolytic infection. CDV proteins or viral nucleocapsids were only very rarely found in oligodendrocytes in culture, in contrast to astrocytes and microglial cells which easily support CDV infection. Thus, we concluded from these studies in vivo and in vitro that CDV causes a restricted infection of the oligodendrocyte, which is possibly responsible for the phenomenon of demyelination. Why the production of viral protein does not take place in these cells remains to be clarified.
The oligodendrocytes, the myelin producing cells loose their specialised functions
Between 20 and 30 days p.i., cultured oligodendrocytes, which grow superimposed on a layer of astrocytes in mixed dog brain cell cultures, start to degenerate and disappear although the supporting culture remains a continuous cell sheet. Ultrastructural studies revealed microvacuolation and loss of organelles in such oligodendrocytes. The morphological changes are preceded by metabolic dysfunction of these cells, because cerebroside sulfo transferase activity--an oligodendrocyte specific enzyme--decreased markedly soon after infection and myelin transcription is strongly decreased in infected brain cell cultures. In vivo we showed that CDV infection led to a massive downregulation of myelin gene transcription. The fate of these oligodendrocytes remains unclear; there is no concrete evidence that these cells undergo necrosis or apoptosis. There is little doubt that a change of these cells lies at the base of the demyelinating process but its mechanism is not yet understood. It is possible that viral transcription taking place in these cells interferes with specialized functions necessary to maintain myelin membranes. It cannot be excluded that these cells are affected as a result of virus-induced changes in other cell types. However, a series of experiments could not confirm this hypothesis. Supernatants derived from CDV infected DBCC did not induce oligodendroglial lesions in recipient dog or mouse brain cultures. We were unable to find evidence for toxic factors such as TNF alpha or reactive oxygen radicals in the supernatants of CDV infected DBCC. Cocultivation of infected DBCC with mouse brain cultures, which are refractory to CDV, did not damage the mouse oligodendrocytes (unpublished results). Likewise, the mouse brain cells, which remained uninfected in these cocultivation experiments, did not provide protection for the canine oligodendrocytes.
In summary, the acute CDV infection of the white matter results in metabolic oligodendroglial changes which leads to demyelination. Whether the change of the oligodendrocyte is the direct result of the restricted CDV infection, which has been shown in these cells, remains to be shown.
There is activity of the immune system despite immuno-suppression
The contribution of the immune response to early lesion development is not clear. While an effective anti-viral neutralizing immune response is lacking in the acute phase of distemper, anti CDV IgM antibodies occur within the first 2 weeks of infection. Despite severe immunosuppression and lack of perivascular cuffing, numerous CD8+ cells are found in acute demyelinating lesions and also diffusely distributed in the brain parenchyma, roughly correlating with areas of viral infection. In the CSF of such animals, high IL8 titers are found. It was suggested that initial microglial cell activation which occurs in distemper may trigger invasion of T cells in the CNS. Indeed, ex vivo cultivation of microglial cells from dogs with nervous distemper showed that these cells are greatly activated. This is further supported by marked MHCII upregulation in macrophages as reported by others. In addition, there is marked upregulation of pro-inflammatory cytokines whereas anti-inflammatory cytokines remain stagnant. Metalloproteinases which regulate blood brain barrier function are also increased. Antiviral cytotoxic immune reactions have only been shown in the later stage of the disease. It is uncertain therefore, whether the invading T cells have any effect at all on infected cells.
| Figure 1. Summary of pathogenesis of demyelination in distemper | 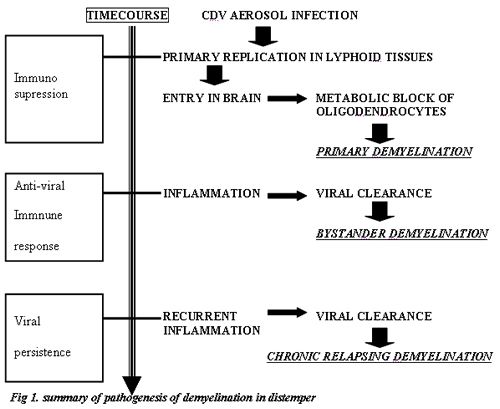
|
|
| |
The chronic stage of distemper: inflammation makes things worse
Coinciding with the recovery of the immune system, perivascular cuffing with lymphocytes, plasma cells and monocytes occurs in the initial virus-induced brain lesions. The inflammatory reaction in the demyelinating lesions can lead to progression of the tissue damage. There is often frank necrosis of the tissue in such lesions. Thus, the chronic stage of the disease is characterized by immuno-pathologic complications.
Is inflammatory demyelination an autoimmune process?
Antimyelin antibodies in serum have been known to occur in distemper since a long time. We found such antibodies also in the CSF of dogs with distemper and that these antibodies are locally produced in the inflammatory brain lesions. A cell-mediated response against myelin basic protein (MBP) was found in 4 of 11 dogs experimentally infected with CDV. However, neither antimyelin antibodies nor cell mediated antimyelin reactions correlate with the course of the disease. In addition, distemper has no resemblance to experimental allergic encephalitis.
Is tissue destruction caused by the antiviral immune response?
The initial intrathecal immune response in distemper during the immunosuppressive stage of the disease consists of diffuse invasion of CD8+ T cells. During immune recovery a mature immune reaction develops by perivascular infiltration of CD4+ cells and subsequent recruitment of large numbers of plasma cells and strong antibody synthesis. The titers of CDV neutralizing antibodies in the CSF often exceed those in the serum. Binding studies show that antibodies are made against all proteins of CDV. The occurrence of anti-CDV antibodies in the CSF coincided with clearance of CDV--and CDV containing cells--from the inflammatory lesions.
We found that in brain cell cultures, antiviral antibodies bound to the surface of CDV infected cells interacted with the Fc receptors of neighbouring macrophages by way of their Fc portions. This interaction resulted in a respiratory burst of the macrophages with release of reactive oxygen radicals. We could also show that stimulation of macrophages by way of their Fc receptors or other means including antiviral antibody--virus immune complexes led to selective destruction of oligodendrocytes in their vicinity. Thus, these experiments showed how the humoral antiviral immune response could lead to destruction of oligodendrocytes as "innocent bystander" cells. Obviously, several products secreted by stimulated macrophages, including reactive oxygen radicals can be made responsible for damage to the oligodendrocyte/myelin compartment. Chemically produced reactive oxygen radicals in the xantine/xantine-oxydase system, which was added to the culture supernatant, selectively damaged cultured oligodendrocytes which are rich in iron compounds, rendering these cells particularly vulnerable to oxygen radical attacks. The procoagulant activity of macrophages was markedly enhanced after CDV infection which may enhance the destructive potential of macrophages and provide further support for the hypothesis that bystander demyelination occurs in chronic distemper. The experimental conditions in the antibody experiments in vitro closely mimic the situation in vivo in which CDV infected glial cells in the white matter are in close contact with macrophages and antiviral antibody producing cells. Therefore, it is not unreasonable to conclude that a bystander mechanism associated with the antiviral immune response can be made responsible for the progression of demyelinating lesions in the chronic stage of CDV infection.
The disease doesn't stop: the virus manages to stay in the brain
The antiviral immune response should be beneficial to the host: we could clearly demonstrate that CDV is removed from the tissue in the inflammatory lesions. However, our studies also showed that CDV can persist in white matter areas outside of the inflammatory demyelinating lesions. It appears therefore that a chronic progressive disease develops if the intrathecal immune response keeps lagging behind viral replication. Thus viral persistence is the key to the pathogenesis of the chronic lesion. We found that persistent CDV spreads in a non-cytolytic manner by way of cell processes with very limited budding and release of infectious virus as compared to attenuated viruses. In contrast to attenuated CDV, virulent CDV also induces very little cell cell fusion, which eventually leads to cell destruction. In addition, CDV is capable to produce a restricted infection in neurons without expressing viral protein. Others have found a restricted expression of surface proteins in the CNS. Thus CDV appears to do everything to avoid being recognized by the immune system. It appears that both the limited shedding of infectious virus and lack of cell-cell fusion is related to a restricted expression of fusogenic complexes in the cell membrane. The responsible molecular determinants of the viral fusion protein are being characterized in our lab.
Treatment and prevention
Much has been learned about the development of the CNS lesions in distemper. Some of these findings may provide a base for the development of therapeutic strategies in particular at the immuno modulatory level. However, while modification of the detrimental inflammatory response may become feasible, the basic problem remains the presence of the virus in the CNS. Effective antiviral therapies against Morbilli viruses are not available yet. Therefore, the most important veterinary intervention remains prevention. Whereas vaccines against CDV have been available since a long time and have greatly reduced the incidence of the disease, avianized strains may offer inadequate protection against the nervous form of CDV and other vaccine strains may cause post vaccinal encephalitis. Recently we have developed a DNA vaccine derived from virulent CDV sequences. Preliminary studies have shown that this vaccine is capable to protect dogs against the clinical manifestations of the infection.