Daniel J. Fletcher
Overview of the Issue
Veterinary practices should be well prepared for early recognition of cardiopulmonary arrest (CPA) and in the practice of cardiopulmonary resuscitation (CPR). Studies in human medicine have shown that a combination of didactic CPR training and opportunities to practice skills are most effective. Training is recommended for all veterinary personnel who may be called upon to assist in a crisis. Refresher training and drills at least every six months have been shown to improve performance in human medicine. Early CPR is critical in patients with CPA to maximize the chance of return of spontaneous circulation (ROSC) and survival.
Objectives of the Presentation
- Demonstrate correct chest compression technique for a dog or cat, given a description of the patient’s chest conformation and size.
- Demonstrate correct mouth-to-snout ventilation technique for a dog or cat in CPA and explain how your approach would differ if the animal were endotracheally intubated.
- Explain the rationale behind the ALS interventions you would use to treat a patient in asystole or pulseless electrical activity (PEA) and contrast them to the ALS interventions you would use to treat a patient with ventricular fibrillation (VF) or pulseless ventricular tachycardia (PVT).
Basic Life Support
Circulation—Chest Compressions
The initial goals of chest compressions are to provide (1) pulmonary blood flow for oxygen uptake and CO2 elimination and (2) tissue perfusion for oxygen delivery to restore cellular metabolic activity. Experimental evidence suggests that even well-executed external chest compressions produce, at best, 30% of normal cardiac output, making proper technique critical. Chest compressions should be started as soon as possible after diagnosis or suspicion of CPA. A delay in the start of high-quality chest compressions reduces the likelihood of return of spontaneous circulation (ROSC).
Chest compressions should be done with the patient in lateral recumbency to a depth of 1/3 to 1/2 the width of the chest at a rate of 100–120 compressions per minute. Leaning on the chest between compressions must be avoided. Chest compressions should be delivered in uninterrupted cycles of two minutes, and a new compressor should take over after each cycle to reduce the effect of rescuer fatigue.
The cardiac pump theory is based on the concept that the left and right ventricles are directly compressed, while the thoracic pump theory is based on the concept that external chest compressions raise overall intrathoracic pressure.
Blood flow generated by the thoracic pump mechanism likely predominates in large dogs with a round-chested conformation. Therefore, it is recommended that the chest be compressed over the highest point on the lateral thoracic wall with the patient in lateral recumbency. In keel-chested dogs, compressions directly over the heart are recommended. In flat-chested dogs (e.g., English bulldogs), compressions over the sternum with the patient in dorsal recumbency may be more effective. In these patients, compressions should not exceed ¼ the depth of the chest. The compressor should maintain locked elbows with one hand on top of the other, and the shoulders should be directly above the hands. This allows compressions to be done using the core muscles. Chest compressions should be done in cats and small dogs (<7 kg) directly over the heart.
Airway and Breathing—Ventilation
The patient should be intubated as soon as possible. Both dogs and cats can be intubated in lateral recumbency, so chest compressions should continue during intubation. If an endotracheal tube is not readily available, mouth-to-snout ventilation is warranted. The patient’s mouth should be held closed firmly with one hand. The neck is extended to align the snout with the spine, opening the airway as completely as possible. The rescuer makes a seal over the patient’s nares with his/her mouth and blows firmly into the nares to inflate the chest. Thirty chest compressions should be delivered, immediately followed by two breaths. Alternating compressions and ventilations should be continued for two-minute cycles, and the rescuers should rotate every cycle to prevent fatigue. Chest compressions and ventilations should be performed simultaneously in intubated patients. Intubated patients should be ventilated at a rate of 10 breaths per minute with an inspiratory time of approximately one second.
Advanced Life Support
Monitoring
Many commonly employed monitoring devices are of limited use during CPR due to their susceptibility to motion artifact and the likelihood that decreased perfusion will compromise accurate readings. Low-yield monitoring devices include pulse oximeter and indirect blood pressure monitors, including Doppler and oscillometric devices. The two most useful monitoring devices during CPR are the electrocardiogram (ECG) and end-tidal CO2 monitor (ETCO2).
An accurate rhythm diagnosis is essential to guide drug and defibrillation therapy. The goal of ECG monitoring during CPR is to diagnose which of the four most common arrest rhythms are present: (1) asystole, (2) PEA, (3) VF, or (4) PVT. Rhythms 1 and 2 are “non-shockable,” and rhythms 3 and 4 are “shockable.” The ECG should be quickly evaluated while compressors are being rotated between two-minute cycles of CPR, the rhythm diagnosis should be called out, and differing opinions should be solicited. Discussion should not prevent rapid resumption of chest compressions.
The presence of measurable CO2 by ETCO2 monitoring is supportive of (but not definitive for) correct placement of the endotracheal (ET) tube. Because ETCO2 is proportional to pulmonary blood flow, it can also be used as a measure of chest compression efficacy under conditions of constant quality of ventilation. An ETCO2 target of 18 mm Hg at a minimum is consistent with adequate chest compression quality. Upon return of spontaneous circulation (ROSC), ETCO2 dramatically increases due to the rapid increase in circulation and, therefore, is a valuable early indicator of ROSC during CPR.
Drug Therapy
For non-shockable rhythms, vasopressors are recommended to increase peripheral vasoconstriction. Because cardiac output is low even during optimal external chest compressions, shunting blood away from the periphery is essential to maintain perfusion to the core. Epinephrine acts via α1 receptors but has β1 and β2 effects. The α1 effects have been shown to be the most beneficial during CPR. Standard dose (0.01 mg/kg IV/IO every other cycle of CPR) is recommended. While previous guidelines suggested high-dose epinephrine for prolonged CPA, this is no longer recommended in the RECOVER 2.0 guidelines. Epinephrine may also be administered via ET tube (0.02 mg/kg) by feeding a long catheter through the ET tube. Vasopressin is an alternative that acts via peripheral V1 receptors.
Atropine is a parasympatholytic drug that has shown some benefit in only a few studies. Atropine at a dose of 0.04 mg/kg IV/IO may be considered during CPR in dogs and cats, especially if there is evidence of increased vagal tone prior to the arrest. The RECOVER 2.0 guidelines recommend only a single dose of atropine as early as possible and no longer recommend repeating atropine due to its long half-life.
Although specific evidence of efficacy is not available, the use of reversal agents in dogs and cats in which reversible anesthetic/analgesic drugs were recently administered may be considered.
Electrical Defibrillation
Defibrillation aims to drive the ventricular myocardial cells into a refractory period, allowing the pacemakers to take over. Defibrillation should be done as soon as possible after diagnosis of a shockable rhythm. Biphasic defibrillators are recommended over monophasic defibrillators because a lower energy is required. For monophasic defibrillators, an initial dose of 4–6 J/kg should be used, while biphasic defibrillation should start at 2–4 J/kg. The second dose may be increased by 100%, but subsequent doses should not be further increased.
After defibrillation, chest compressions should be resumed immediately, and a full two-minute cycle of CPR administered before reassessing the ECG and determining if the patient is still in VF and should be defibrillated again. Brief assessment of the ECG immediately after defibrillation to determine if a perfusing rhythm has resulted is reasonable but should minimally delay the resumption of chest compressions.
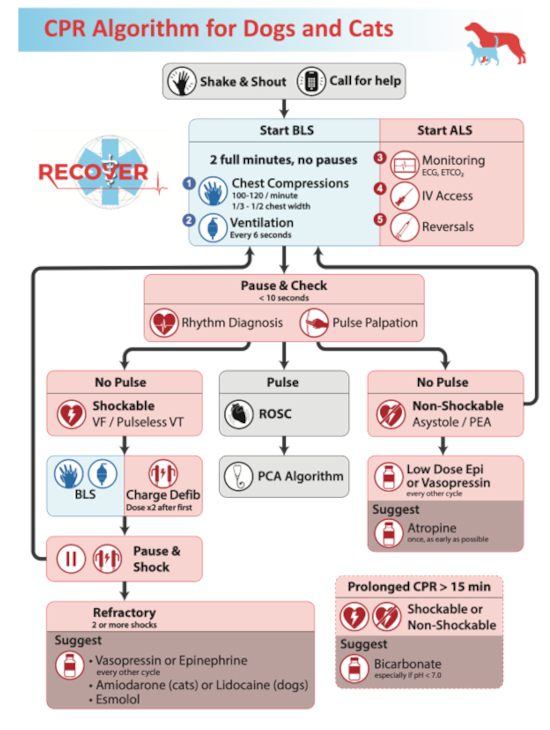
Algorithm
This is a draft of the RECOVER 2.0 CPR algorithm, which summarizes the key points of management of patients during CPR.
Image 1
References
1. Fletcher DJ, Boller M, Brainard BM, et al. RECOVER evidence and knowledge gap analysis on veterinary CPR. Part 7: clinical guidelines. J Vet Emerg Crit Care. 2012;22;Suppl 1S102–31.
2. Hopper K, Epstein SE, Fletcher DJ, et al. RECOVER evidence and knowledge gap analysis on veterinary CPR. Part 3: basic life support. J Vet Emerg Crit Care. 2012;22;Suppl 1S26–43.
3. McMichael M, Herring J, Fletcher DJ, et al. RECOVER evidence and knowledge gap analysis on veterinary CPR. Part 2: preparedness and prevention. J Vet Emerg Crit Care. 2012;22;Suppl 1S13–25.