Nutraceutical Chondroprotectives and Their Use in Osteoarthritis in Zoo Animals
Abstract Introduction
Recently, the result of many years of research that originated primarily in Europe, has led to the development of a new class of nutrients that act completely differently from medications historically used for osteoarthritis. These compounds are collectively termed chondroprotective agents, since they directly affect chondrocytes in a beneficial manner.
As zoo animal management and health care improve, zoo veterinarians are faced with managing an increased number of geriatric patients. Osteoarthritis is a prevalent cause of morbidity in these patients. The Los Angeles Zoo has a large percentage of geriatric animals. A review of the mammal collection in 1996 showed 20% were considered to be geriatric, and 50% were past breeding age. A review of the last 4 yr of medical entries showed 60 cases in mammals of geriatric osteoarthritis treated by clinicians with therapies including chondroprotectives. Success of treatment can be subjective, however caretakers and veterinarians felt they saw improvement in the majority of cases. The method of action for the chondroprotective agents, common product examples, the data supporting their use, and three case studies from the Los Angeles Zoo are presented.
Methods of Action and Products
Normal articular cartilage consists of chondrocytes (10%) surrounded by an extracellular matrix (90%) of water, collagen and proteoglycans. Cartilage is unique among body tissues by being avascular, aneural and alymphatic. All materials necessary for chondrocyte function must diffuse through the matrix from synovial fluid or subchondral bone. This creates diffusion dynamics for the supply of vital nutrients to cartilage that normally is only barely adequate to maintain normal turnover. Thus, any insult can easily affect the nutritional state of cartilage. Such insults result in a need for augmented synthesis that often generates extremely large demands of raw materials. As chondrocytes are lost the ability to increase production is also decreased.
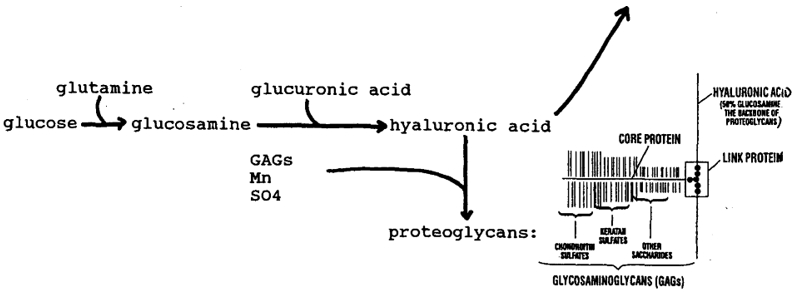
Proteoglycans consist of a core protein with glycosaminoglycan side chains, linked to a hyaluronic acid (itself a glycosaminoglycan) backbone (Figure 1). Glycosaminoglycans (GAGs) are mucopolysaccharides (repeating sugar molecules). There are six types in the body: chondroitin sulfate, keratan sulfate, hyaluronic acid, dermatan sulfate, heparin, and heparan sulfate. The two found in proteoglycan side chains are chondroitin sulfate and keratan sulfate. Hyaluronic acid is made of glucuronic acid and glucosamine and is also a component of synovial fluid, the viscous fluid that bathes the synovial membrane of the cartilaginous joint.
Figure 1. The reaction below occurs in the chondrocyte
Glucosamine:5,10
1. Is a precursor for hyaluronic acid and proteoglycans.
2. Stimulates synthesis of collagen and proteoglycans.
3. Has a mild anti-inflammatory effect.
4. Has no toxicity and excellent bioavailability orally. (Pharmacokinetics have been tested in dogs, rats, and humans.)
Chondroitin:5,10
1. Is a building block of proteoglycans.
2. Inhibits degradative enzymes that destroy cartilage (protects against catabolism of the joint).
3. Prevents fibrinthrombi in synovial or subchondral microvasculature.
4. Has an anti-atherosclerotic effect—maximizes blood circulation to tissues. (Important in common geriatric diseases such as diabetes, heart and renal disease, etc.)
5. Has an anti-inflammatory activity on the cellular level.
6. Has an affinity for articular tissues, is well absorbed orally.
It has also been shown in cell culture that these two nutrients work synergistically by upregulating cartilage metabolism.12
There are many available products containing these supplements:
1. GAGs: Polysulfated GAGs (PSGAGs): Adequan® (Luitpold Pharmaceuticals, Shirley, New York, USA).
2. Mixed GAGs: From freeze dried green-lipped mussel (Perna canaliculus): Glycoflex®, Synoflex® (equine - caramel and cinnamon flavors), Nu-Cat® (feline - has taurine and digestive enzymes). (Vetri-Science Laboratories, Essex Junction, Vermont, USA).
3. Chondroitin/keratan sulfate: From bovine, shark cartilage
4. Glucosamine HCl or sulfate: Derived from crab shells (chitin).
5. Glucosamine HCl/chondroitin sulfates/manganese: Cosequin® - veterinary & Cosamin® - human (Nutramax Laboratories, Baltimore, Maryland, USA). The equine powder has 3:1 ratio of glucosamine to chondroitin sulfate vs. SA is 1:1 due to difference in absorption patterns between carnivores and herbivores.
Products may also contain various minerals and vitamins involved in proteoglycan synthesis (Mn) and creating collagen from amino acids (Fe, Cu, Zn, Mn, vitamin C), free radical scavengers (vitamin C, vitamin E), omega-3 fatty acids for prostaglandin synthesis, etc. Nutraceuticals require no testing and products may or may not actually contain what the label claims.
Studies Supporting Oral Chondroprotective Use
Many species have been studied, primarily humans, horses, rabbits, rats, and dogs. The use of injectable PSGAGs has been well described.2 Oral supplements have been in use in Europe for 30 yr in arthritic people and a large body of European literature exists.
Chondroitin. Studies done with Condrosulf® (IBSA, Lugano, Switzerland), a pure chondroitin 4,6 sulfate European product, showed it to be protective for cartilage insults in rabbits. Human studies showed it to improve knee arthritis, and to be protective for erosive finger lesions in a 3-yr study. When diclofenac sodium, a non-steroidal anti-inflammatory drug (NSAID) was compared to chondroitin in a sixth trial, chondroitin effects lasted 3 mo after stopping but had a later onset, the NSAID caused prompt resolution, but signs reappeared after stopping. Another study showed concomitant use of chondroitin and diclofenac resulted in less pain than with either alone, and patients were able to decrease the NSAID by 72%.3
Perna. A double-blind study with humans in Scotland showed 46–76% efficacy in rheumatoid and osteoarthritis.6
Glucosamine. Studies showed pain relief and increased joint flexibility.14 Onset of action was weeks, but then glucosamine performed the same or better than ibuprofen with no side effects.13,15 Most recently in the United States, Cosequin®/Cosamin® has been studied. In a study with horses, within 2 wk after starting Cosequin® treatment, horses with proven degenerative joint disease (DJD) showed statistically significant clinical improvement irrespective of age, joint affected or use of the horse.8 Another study involving navicular disease showed consistent improvement of Cosequin®-treated horses vs. placebo horses.7 In a study with dogs, animals pre-treated with Cosequin® were protected against experimentally induced synovitis and showed decreased lameness.3 It caused a decrease in post-surgical stifle osteoarthritis in another study.9 Two 1999 Cosamin® studies with humans (one on Navy SEALS) showed relief of DJD knee symptoms with no hematologic effects.4,11 Rabbits showed histologic decreases in moderate and severe cartilage lesions when pre-treated with Cosequin®.16
Case Reports
Forty-two species of mammals at the Los Angeles Zoo have been treated with these products at dosages recommended by the manufacturers (dosed by body weight) (Table 1). Three specific examples are detailed below:
1. Thirteen-year-old (age estimated) wild-caught black howler monkey (Alouatta caraya): Noted to be “slowing down” with a hunched posture, unable to grip with tail normally. Physical exam showed scoliosis of spine; radiographs showed severe ventral bridging spondylosis through T–L region. He was started on Glycoflex® 100 mg p.o., s.i.d. and was much improved within 2 wk, using his tail to prehend and more mobile and active. This persisted for 1.5 yr when he died of chronic renal failure.
2. Ten-year-old (age estimated) wild-caught harnessed bushbuck (Tragelaphus scriptus scriptus): Presented for a right rear lameness and hunched and swinging gait in the rear and a gradual decline in its ability to get up in the morning and move quickly, that it would “warm out of.” One scoop of Cosequin® for two animals over grain once a day was started. After 2 wk, its keeper felt it was improved. Two months later, after attempted breeding by the male, it worsened and was examined: Radiographs of the hip and spine were normal after an initial pop of the right hip on palpation. Three days later the lameness had resolved. Mild signs gradually reappeared and it maintained for another 2.5 yr when it deteriorated and was euthanatized for humane reasons. On necropsy there was histologic confirmation of chronic degenerative arthritis in the right coxofemoral joint.
3. Seventeen-year-old Central American tapir (Tapirus bairdii): History of chronic intermittent right rear leg lameness of greater than 8 yr duration, at times non-weight bearing. Radiographically, no visible joint lesions were seen. He had been managed on soft substrate, with nonsteroidal antiinflammatory drugs when lameness was severe. After 2.5 wk on ½ scoop Cosequin® p.o., b.i.d., his lameness was significantly improved. Over the past 16 mo, his periods of lameness have been much less frequent with no non-weight-bearing episodes. After a recent move to a hard-floored area he has maintained well with one moderate and rapidly resolving period of lameness treated with a short course of NSAIDs in addition to the Cosequin®.
Table 1. Species treated with nutraceuticals at the Los Angeles Zoo
|
Marsupials:
|
Koala
|
Phascolarctos cinerus
|
|
|
Wallaroo
|
Macropus robustus
|
|
|
Kangaroo
|
Macropus giganteus
|
|
Primates:
|
Ring-tailed lemur
|
Lemur catta
|
|
|
Bushbaby
|
Galago crassicaudatus
|
|
|
Black howler monkey
|
Alouatta caraya
|
|
|
Golden-lion tamarin
|
Leontipithecus rosalia
|
|
|
Emperor tamarin
|
Saguinus imperator
|
|
|
Moustached guenon
|
Cercopithecus cephus
|
|
|
Drill
|
Papio leucophaeus
|
|
|
Siamang
|
Hylobates syndactylus
|
|
|
Orangutan
|
Pongo pygmaeus
|
|
Carnivores:
|
Dingo
|
Canis familiaris
|
|
|
Maned wolf
|
Chryocyon brachyurus
|
|
|
Polar bear
|
Ursus maritimus
|
|
|
Wolverine
|
Gulo gulo
|
|
|
Mountain lion
|
Felis concolor
|
|
|
Lion
|
Panthera leo
|
|
|
Snow leopard
|
Panthera uncia
|
|
|
Jaguar
|
Panthera onca
|
|
Proboscideans:
|
Asian elephant
|
Elephas maximus
|
|
Perissodactyla:
|
Donkey
|
Equus asinus
|
|
|
Baird’s tapir
|
Tapirus bairdii
|
|
|
Black rhinoceros
|
Diceros bicornis
|
|
Artiodactyla:
|
Babirusa
|
Babyrousa babyrussa
|
|
|
Warthog
|
Phacochoerus africanus
|
|
|
Guinea hog
|
Sus scrofa
|
|
|
Chinese water deer
|
Hydropotes inermis
|
|
|
Giraffe
|
Giraffa camelopardalis
|
|
|
Pronghorn
|
Antilocapra americana
|
|
|
Bison
|
Bison bison
|
|
|
Giant eland
|
Taurotragus derbianus
|
|
|
Bongo
|
Tragelaphus eurycerus
|
|
|
Bushbuck
|
Tragelaphus scriptus
|
|
|
Black duiker
|
Cephalophus niger
|
|
|
Red-flanked duiker
|
Cephalophus rufilatus
|
|
|
Gerenuk
|
Litocranius walleri
|
|
|
Markor
|
Capra falconeri
|
|
|
Nubian ibex
|
Capra ibex
|
|
|
Domestic goat
|
Capra hircus
|
|
|
Serow
|
Capricornis crispus
|
|
|
Mountain goat
|
Oreamnos americana
|
Conclusion
Osteoarthritis is an irreversible disease and the most effective treatment is prevention. Once it develops however, options for treatment have consisted of surgery, weight reduction, controlled exercise, and pain relief medication. Nonsteroidal and steroidal anti-inflammatory drugs are used as palliative therapy, but can have significant drug side effects. Studies have also shown that these drugs can down-regulate chondrocyte metabolism and actually decrease GAG synthesis.10
Nutraceutical chondroprotective agents might provide another treatment for, and may perhaps prevent osteoarthritis with no apparent side effects. They need to be used early in the process, since they require viable chondrocytes and some cartilage to be effective. Effects may be seen after 2 wk, with full effect taking 6–8 wk. If anti-inflammatory or analgesic medication is needed, they should be used in conjunction. They may decrease the amount required and help prevent the catabolic effects of nonsteroidal antiinflammatory drugs and corticosteroids. Intermittent therapy may be possible and needs further study.
Literature Cited
1. Altman RD, D Uebelhart, G Verbruggen, et al. 1998. Chondroitin Sulfate: Update in osteoarthritis. Osteoarthritis and Cartilage. 6: 1A–46A.
2. Boulay JP, M DeAngelis, SA Kincaid, et al. 1995. Medical therapy of osteoarthritis in dogs. Compendium Supplement: Vet Exchange. 1–19.
3. Canapp SO, RM McLaughlin, JJ Hoskinson, et al. 1998. Scintigraphic evaluation of glucosamine HCl and chondroitin sulfate as treatment for acute synovitis in dogs. Proc. Am. Coll. Vet. Surgeons. P. 5.
4. Das AK, J Eitel, TA Hammond, et al. 1998. Efficacy of a new class of agents (glucosamine HCl and chondroitin sulfate) in the treatment of osteoarthritis of the knee. Proc. Am. Assoc. Hip and Knee Surgeons. P. 49.
5. Davis WM. 1998. The role of glucosamine and chondroitin sulfate in the management of arthritis. Drug Topics. 4: 3S–15S.
6. Gibson RG, SLM Gibson, V Conway, et al. 1980. Perna canaliculus in the treatment of arthritis. The Practitioner. 224: 955–960.
7. Hanson RR, WR Brawner, Hammand TA, et al. 1998. The clinical profile of a glucosamine-chondroitin sulfate compound* in a double-blinded, placebo-controlled, randomized trial as a selective symptom modifying nutraceutical for navicular syndrome: current data and perspectives. Proc. Vet. Orthopedic Society. P. 63.
8. Hanson RR, LR Smalley, GK Huff, et al. 1997. Oral treatment with a glucosamine-chondroitin sulfate compound for degenerative joint disease in horses: 25 cases. Equine Practice. 19: 16–22.
9. Hulse DS, D Hart, M Slatter, et al. 1998. The effect of Cosequin® on cranial cruciate deficient and reconstructed stifle joints in dogs. Proc. Vet. Orthopedic Society. P. 64.
10. Hungerford DS. 1998. Treating osteoarthritis with chondroprotective agents. Orthopedic Special Edition. 4:1.
11. Leffler CT, AF Philippi, SG Leffler, et al. 1999. Glucosamine, chondroitin, and manganese ascorbate for degenerative joint disease of the knee or low back: a randomized, double-blind, placebo-controlled pilot study. Military Medicine. 164: 85–91.
12. Lipiello L, A Idouraine, PS McNamara, et al. 1999. Cartilage stimulatory and antiproteolytic activity is present in sera of dogs treated with a chondroprotective agent. Canine Prac. 24: 18–19.
13. Muller-Fasbender H, GL Bach, W Haase, et al. 1994. Glucosamine sulfate compared to ibuprofen in osteoarthritis. Osteoarthrit. Cart. 2: 61–69.
14. Noack W, MF Fischer, KK Forster, et al. 1994. Glucosamine sulfate in osteoarthritis of the knee. Osteoarthrit. Cart. 2: 51–59.
15. Vaz AL. 1982. Double-blind clinical evaluation of the relative efficacy of ibuprofen and glucosamine sulfate in the management of osteoarthrosis of the knee in out-patients. Cur. Med. Res. Opin. 8: 145.
16. Woodward JR, L Lipiello, R Karpman, et al. 1999. Beneficial effects of a dietary chondroprotective agent in a rabbit instability model of osteoarthritis. Proc. Am. Academy of Orthopedic Surgeons Paper. 48.