L. Findji
Climbing up the "ladder" of reconstruction techniques (cf. "Skin Reconstruction: Basic Techniques"), when simple primary closure is not possible and no local flaps are available to cover a wound, axial pattern flaps should be considered. If no axial pattern flap is deemed suitable, appropriate distant flaps and free skin grafts should next be sought. This second part will focus on axial pattern flaps, distant flaps and free skin grafts.
Axial Pattern Flaps
Skin flaps are either subdermal (relying on the subdermal vascular plexus) or axial (relying on a direct cutaneous artery).
Axial pattern flaps are determined by the area of skin vascularised by a major direct cutaneous artery (angiosome), after which it is named (Figure 1a). Many direct cutaneous arteries which can be used to perform axial flaps have been described. Provided this artery is preserved, such flaps are more robust and survive on greater lengths compared to equivalent subdermal flaps. They can even be islanded (i.e., entirely cut out from the donor site apart from their vascular pedicle [Figure 1b]). However, axial flaps cannot be elevated in any direction: their design has to follow the description of the cutaneous area vascularised by the chosen direct cutaneous artery. The anatomical landmarks of each axial pattern flap are provided in their original description and in textbooks. The most commonly used axial flaps include the caudal superficial epigastric, thoracodorsal, omocervical, deep circumflex iliac and caudal auricular flaps.
| Figure 1. Vascularisation of axial flaps | 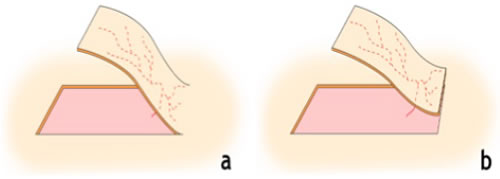
Peninsular flap (a), island flap (b) |
|
| |
Skin flaps, either subdermal or axial, are transposed with their own vascularisation and can survive on poorly vascular beds or over cavities.
Distant Flaps
Distant flaps are subdermal flaps which can be used for reconstruction of wounds on limb extremities (distal to the elbow or stifle). Ideally, the wound, or at least part of it, is lateral. Extensive, circumferential wounds (degloving injuries) are very good indications. With these flaps, the wound is taken to the excess skin rather than the other way round, like in other flaps. With distant flaps, the reconstruction is by necessarily staged, as their principle is to give enough time for a vascularised portion of skin to heal on the wound to reconstruct, sufficiently to be secondarily detached from the trunk and survive on its neovascularisation from the wound. These flaps include hinge and pouch flaps, depending on whether a monopedicular or a bipedicular subdermal flap is elevated on the trunk. Pouch flaps ("tunnelisation") are safer both because of their double pedicle and because they immobilise the leg better. The disadvantages of these flaps are to require that the patient tolerate having the treated leg maintained against the trunk during the first phase of the reconstruction. Very heavy patients or patients with severe orthopaedic issues of the remaining limbs may not be good candidates for this technique. In any case, a degree of ankylosis is expected when the leg is released, but usually resolves spontaneously or with minimal physiotherapy.
To perform a distant flap, the leg to treat is brought to the trunk and a skin flap is elevated from the trunk to cover the wound. This is left to heal 7–18 days depending on the age of the dog and whether the flap is released from the trunk progressively or not. If a circumferential wound is to be covered, enough skin is harvested from the trunk to be wrapped around the released leg and cover the medial aspect of the wound. If the wound to reconstruct is large, closure of the donor site may itself require the use of skin flaps.
Free Skin Grafts
Skin grafts consist of transposing free portions of skin to a wound. The transposed skin is therefore no longer perfused and relies on the development of a neovascularisation from the receiving bed for survival. The receiving bed must therefore be healthy and well vascularised, so that sufficient neovascularisation can develop from it.
Graft can be harvested as full-thickness (epidermis and entire dermis) or partial-thickness (epidermis and variable portions of dermis). In practice, harvesting partialthickness grafts in dogs and cats is technically difficult without dedicated devices (dermatome). In consequence, only full-thickness grafts will be discussed here.
Graft Types
In veterinary surgery, full-thickness grafts, harvested from the ventrolateral portions of the trunk, are most commonly used. Different forms of grafts exist: meshed, unmeshed, pinch, punch and strip grafts.
Punch grafts are harvested with a punch biopsy instrument. Matching-size holes are created in the granulation tissue of the recipient bed to accommodate the grafts. The main advantages of these grafts are that they are easy to perform, allow very good drainage of the wound and withstand infection better than other types of graft. However, the resulting cosmetic aspect is rather poor.
Meshed and unmeshed grafts use a single skin portion to cover the recipient bed. Meshed grafts are obtained by creating incisions throughout the graft. These incisions allow postoperative drainage, which favours graft adhesion and survival, and enable grafts to cover greater areas compared to unmeshed grafts of similar size. Meshed grafts can be prepared manually or with a dedicated device, which produces more even and expandable meshes, but relying more on secondintention healing and therefore possibly resulting in a poorer cosmetic result. The author almost exclusively uses meshed full-thickness free skin grafts.
Principles of Free Skin-Grafting Techniques
A free skin graft is transferred without any vascular supply and therefore relies on the rapid development of neovascularisation from the recipient bed, which should either be a healthy granulating wound or a fresh, well-vascularised surgical wound. Every effort must be made to minimise the time required for new vessels to grow from the recipient bed to the dermis of the graft. The hypodermis is removed from the graft as thoroughly as possible before it is placed on the recipient bed, on which the graft must be tacked as much as possible. Tacking the graft minimises the gap new vessels have to cross to reach the dermis, prevents movements of the graft relative to the recipient bed which would impair neovascularisation and avoids accumulation of any fluid interface (seroma, blood) between the graft and the recipient bed. The applied graft must also be immobilised and any fluid which may accumulate between the graft and the recipient bed must be drained and absorbed. A bandage is placed aseptically at the end of surgery and is left unchanged for 3 to 5 days, to avoid disrupting the graft in the early, critical stages of its adhesion on the recipient bed. The utilisation of vacuum-assisted wound closure (VAC) for a few days after surgery was recently shown to increase the surviving proportion of free skin-grafts in dogs. The bandage is first changed with extreme care 3 to 5 days after surgery, under general anaesthesia or deep sedation, depending on the compliance of the patient.
The aspect of the graft can be variable and appear concerning during the first week after surgery. It can be either pale or dark, before becoming pink again. Consequently, unless the graft is clearly necrotic, it should not be touched regardless of its aspect, and bandage changes must be continued every 2 to 4 days, as needed. In most cases, the aspect of the graft will improve as it takes, at least partially.