Assistant Professor of Anesthesiology, Small Animal Clinical Sciences, Texas A&M University, College Station, TX, USA
One of the leading causes for perioperative deaths in small animal practice is a result of poor oxygen delivery to tissues from cardiac pump failure or vascular collapse.1 Blood pressure monitoring is of utmost during the perioperative period when diagnosing these problems. Invasive or noninvasive blood pressure monitoring is a common modality used when assessing for adequate perfusion of tissues. Invasive (direct) blood pressure monitoring is considered the gold standard and involves arterial catheterization, a pressure transducer, and a specialized monitor. Noninvasive (indirect) blood pressure monitoring through the use of a Doppler or oscillometric systems are commonly performed in routine practice but has their limitations in terms of accuracy.
Definition of Blood Pressure
Arterial blood pressure is a factor of cardiac output (heart rate x stroke volume) and systemic vascular resistance (Figure 1). Stroke volume is determined by preload, afterload, and contractility. Intravascular volume which affects preload primarily, is just one of several causes that may alter blood pressure. Hypotension was been recently defined by both ACVAA and ECVAA diplomats as a systolic or mean arterial blood pressure less than 87±8 mm Hg or 62±4 mm Hg, respectively.2 In the same survey, treatment for hypotension was determined when systolic or mean arterial blood pressure was less than 85±11 mm Hg or 61±8 mm Hg, respectively. Untreated hypotension can lead to organ ischemia, organ damage or failure, and even patient mortality.
| Figure 1. Mechanisms and causes of hypotension | 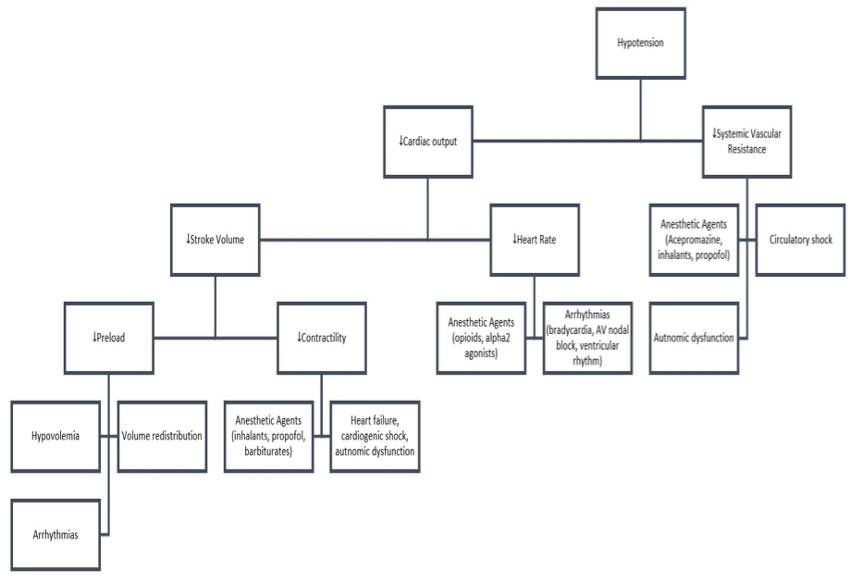
(Extrapolated from Klabunde RE. Cardiovascular integration, adaptation, pathophysiology. In: Klabunde RE, ed. Cardiovascular Physiology Concepts. 2nd ed. Baltimore: Lippincott Williams & Wilkins Co; 2012:206.) |
|
| |
During State of Hypotension, Why Not Intravenous Fluids?
Due to the many factors that contribute to blood pressure, fluid therapy may not always be the most appropriate treatment. Especially in normovolemic patients that are hypotensive. Identifying the cause for hypotension is required in order to provide optimal therapy. Patients that are hypotensive from primary cardiogenic causes and administrated intravenous fluids could further deteriorate by developing pulmonary edema. During the intraoperative period, it has been reported that high-volume and rapid rate administration of isotonic crystalloids was ineffective in counteracting isoflurane-induced hypotension in normovolemic dogs.3 This is most likely as a result of isoflurane's effect on vascular resistance and contractility rather than intravascular volume. Unnecessary administration of fluids may also result in hemodilution, decreases in oncotic pressure, and altered electrolytes potentially increasing patient morbidity.3-5 The objective of this lecture is to discuss the causes and goal-directed therapy of hypotension.
Causes and Treatments of Hypotension
Common causes of hypotension during anesthesia includes bradycardia, hypovolemia, vasodilation, and decreased myocardial contractility.6 Figure 1 depicts some mechanisms and causes of hypotension. As stated previously, there are many causes for hypotension and not all are associated with decreases in intravascular volume and warrant increased intravenous fluid administration as therapy. It is important to treat the underlying source appropriately.
Decreases in systemic vascular resistance (vasodilation) resulting in hypotension during the perioperative period can be a result of anesthetic agents (acepromazine, inhalants, propofol, thiopental, alfaxalone), anaphylaxis, severe acidosis or alkalosis, electrolyte abnormalities, sepsis, SIRS, and hypoxia. Treatment should be focused on the primary cause. Vasopressors may also be used to reduce vasodilation and thereby increasing blood pressure. Phenylephrine infusions, high-dose dopamine infusions, or boluses of ephedrine may be used as first-line therapy during vasodilatory hypotension. Dopamine and ephedrine may also increase heart rate and contractility. A norepinephrine infusion would be considered a good second choice if these agents fail to increase blood pressure. The financial cost of norepinephrine is what limits its use in many practices. Finally, epinephrine or vasopressin infusions can be used as a last resort in non-responsive hypotensive cases. Epinephrine or vasopressin are not routinely used as first-line agents as they possess extreme vasoconstrictor properties and in certain states may decrease perfusion to organs.
Bradycardia is considered when the heart decreases <50% of what is considered normal for that breed or species. Intraoperatively bradycardia is also considered a 50% reduction in heart rate from baseline values (prior to premedication). Bradycardia may be a result of anesthetics (opioids, α2 agonist), hypothermia, hypothyroidism, increased vagal tone (GI disease, respiratory disease, oculocardiac reflex), and cardiac disease. Similar to treating vasodilation the underlying cause should be corrected to the best of the clinician's ability. Core body temperature of less than 97°F or 36°C causes a decrease in spontaneous depolarization in atrial pacemaker cells resulting in bradycardia. Passive warming or the use of external heating devices can increase body temperature and therefore heart rate. Opioids and α2 agonist doses can be reduced or reversed with naloxone or atipamezole, respectively. When analgesia is required the clinician should avoid reversing opioids, but instead administer an anticholinergic. Anticholinergics such as atropine or glycopyrrolate are agents of choice when treating bradycardia. In the author's experience, when additional anticholinergics are required following an initial dose, the latter dose should be reduced by 50%–75% to avoid iatrogenic tachycardia. Ketamine in dogs and cats or alphaxalone in dogs can be considered as induction agents in bradycardic patients as they are shown to increase heart rate.
Decreased contractility inducing hypotension may be a result of cardiac disease, anesthetic agents (inhalants, propofol, and barbiturates), electrolyte abnormalities, hypoxia, severe acidosis or alkalosis, and sepsis. Positive inotropes that are commonly administered perioperatively include dobutamine, dopamine, and ephedrine. These agents stimulate β1 receptors in the cardiac muscle. The administration of drugs such as opioids, benzodiazepines, dexmedetomidine (low dose), and ketamine during that perioperative period can reduce the amount of inhalants or propofol required and therefore minimize decreases in contractility. In healthy patients, ketamine indirectly improves cardiac output (increases heart rate) and blood pressure via the release of catecholamines. However, in patients depleted of catecholamines, for example as seen during sepsis, ketamine will directly decrease contractility and may further exacerbate hypotension.
Hypovolemia can also lead to hypotension and may be a result of dehydration, hemorrhage, Addisonian crisis, gastrointestinal disease, burns, diarrhea, vomiting, diuretics, and inadequate fluid intake. Inadequate intravascular volume can lead to decreases in preload and therefore cardiac output. Volume resuscitation is of utmost importance and can be achieved through the administration of crystalloids, colloids, hypertonic saline, and/or blood products when indicated. Blood work, physical exam, blood pressure monitoring, and a pulse oximeter may aid in diagnosing hypovolemia. Variations in amplitude of the pulse waveform on the pulse oximeter's plethysmograph during positive pressure ventilation may be an indicator of hypovolemia. This is a result of decreases in venous return as the lungs inflate and collapse the major veins leading to the heart. This time of variation occurs commonly in hypovolemia patients, but rarely in normovolemic patients. Blood pressure monitoring may not be the best indicator in assessing a response to fluid administration.7 In hypotensive dogs, cardiac output increased with fluid administration, but not always blood pressure.7 This makes it difficult when evaluating fluid therapy at times. A practitioner should always consider other parameters such as heart rate, lactate, capillary refill time, and pulse quality in addition to blood pressure when assessing response the fluid administration.
Conclusion
Hypotension is a result of many factors and not all of which are responsive to fluid therapy. Fluid therapy should be reserved for those that require intravascular volume resuscitation. Positive inotropes, positive chronotropes, and vasopressors are recommended when decreases in contractility, heart rate, and vascular resistance occur, respectively. The use of intravenous fluids may increase patient morbidity and mortality when not indicated or inappropriately used.
References
1. Brodbelt D. Perioperative mortality in small animal anaesthesia. Vet J. 2009;182(2):152–161.
2. Ruffato M, Novello L, Clark L. What is the definition of intraoperative hypotension in dogs? Results from a survey of diplomates of the ACVAA and ECVAA. Vet Anaesth Analg. 2015;42(1):55–64.
3. Valverde A, Gianotti G, Rioja-Garcia E, Hathway A. Effects of high-volume, rapid-fluid therapy on cardiovascular function and hematological values during isoflurane-induced hypotension in healthy dogs. Can J Vet Res. 2012;76(2):99–108.
4. Wright BD, Hopkins A. Changes in colloid osmotic pressure as a function of anesthesia and surgery in the presence and absence of isotonic fluid administration in dogs. Vet Anaesth Analg. 2008;35(4):282–288.
5. Orbegozo Cortes D, Rayo Bonor A, Vincent JL. Isotonic crystalloid solutions: a structured review of the literature. Br J Anaesth. 2014;112(6):968–981.
6. Hunyady KG, Johnson RA. Anesthesia case of the month. Hypotension. J Am Vet Med Assoc. 2006;229(8):1250–1253.
7. Muir WW, Ueyama Y, Pedraza-Toscano A, Vargas-Pinto P, Delrio CL, George RS, et al. Arterial blood pressure as a predictor of the response to fluid administration in euvolemic nonhypotensive or hypotensive isoflurane-anesthetized dogs. J Am Vet Med Assoc. 2014;245(9):1021–1027.