Clarke Atkins, DVM, DACVIM (Internal Medicine and Cardiology); Jane Lewis Seaks, Distinguished Professor Emeritus
College of Veterinary Medicine, North Carolina State University, Raleigh, NC, USA
Heart sounds are produced by valve movements and the resultant vibrations in the heart, vascular walls, and blood columns. In the normal dog and cat, heart sounds that are typically audible include S1 ("lub") and S2 ("dub") (Figure 1). S1, which is associated with closure of the atrioventricular (mitral and tricuspid) valves, is louder, longer, and of lower pitch than S2, and is best heard over those valve regions (M and T) indicated in Figures 2 and 3. S1 becomes louder with exercise, excitement, or anemia and varies with heart rate and PR interval. The intensity of S1 also varies with atrial fibrillation, atrial or ventricular premature beats, or marked sinus arrhythmia. S2 coincides with semilunar (aortic and pulmonic) valve closure and is best heard over the valve locations (A and P) indicated in Figure 2. The intensity of S2 may increase with pulmonic stenosis, heartworm disease, hyperthyroidism, or pulmonary or systemic hypertension. The intensity is decreased in cardiogenic shock. In normal dogs and cats, S3 (produced by vibrations associated with rapid ventricular filling) and S4 (produced by atrial systole) are not audible (Figure 1). These sounds, termed cardiac gallops, are however, detectable in certain disease states.
| Figure 1 | 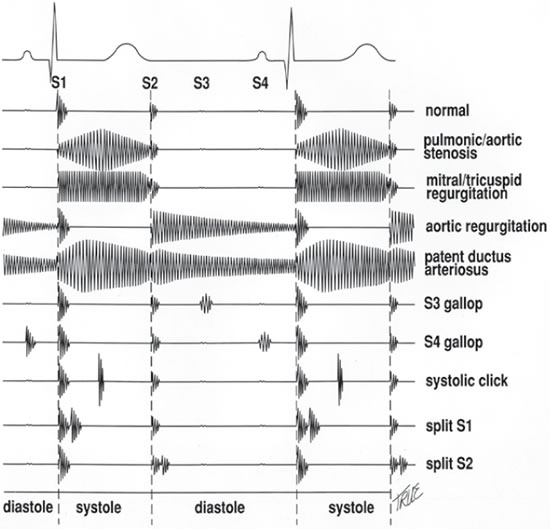
|
|
| |
| Figure 2 | 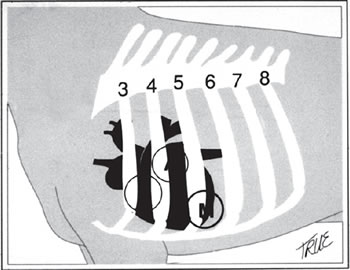
|
|
| |
| Figure 3 | 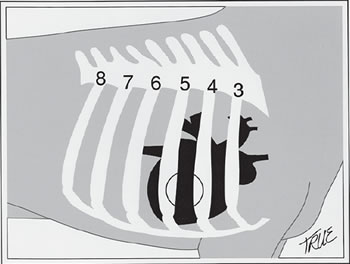
|
|
| |
Abnormal heart sounds offer the veterinarian an indication of the presence of cardiac disease, as well as specific information as to the underlying diagnosis. In some, but not all, instances, abnormal heart sounds give some indication of the severity of the underlying lesion. Careful auscultation, along with information obtained from the remainder of the physical examination, history, and ancillary diagnostic procedures, provides the means by which a specific diagnosis of cardiac disease is made. It should be kept in mind that, in some instances (e.g., anemia), abnormal cardiac sounds do not represent organic heart disease.
Ideally, auscultation of the heart should be performed in a quiet room, with a standing, cooperative patient. Usually the more dramatic heart sounds are evaluated after listening to the more subtle respiratory sounds. A stethoscope is placed over each heart valve (Figure 2) in turn, as well as over the carotid arteries and other areas of interest. The stethoscope's diaphragm is pressed firmly to the thorax to maximize high-frequency sounds, while the bell portion is lightly applied, maximizing low-frequency sounds such as cardiac gallops.
Auscultation is but one portion of the cardiac examination. Palpation of the femoral pulse provides additional information as to pulse quality and strength and, hence, blood pressure and tissue perfusion. Simultaneous auscultation and pulse palpation aids in the detection of pulse variability and deficits, indicating arrhythmias. Information on tissue perfusion, presence of cyanosis, the state of hydration, and the status of the erythron can be obtained by examination of the mucous membranes. The finding of peripheral venous distension or the presence of ascites is compatible with right heart failure. Auscultation of the respiratory tract may reveal adventitious lung sounds compatible with pulmonary edema of left heart failure or concurrent respiratory disease. Thoracic malformation, cardiac hyperkinesis and enlargement, precordial thrill (palpable murmur), or abnormal cardiac position may be revealed by thoracic palpation, while thoracic percussion is employed to detect pleural effusion.
Causes, Pathophysiology and Clinical Signs
Abnormal heart sounds are divided into several categories: murmurs, abnormal splitting of heart sounds, gallops (audible S3 or S4), clicks, friction rubs, audible arrhythmias, and muffled heart sounds. Of these, only cardiac gallops and friction rubs are consistently associated with heart disease.
Murmurs
Heart murmurs (Figure 1) result when turbulence is produced within the heart or vessels by abnormalities in size of vascular or valve orifices, abnormal communications, and alterations in blood velocity and viscosity. The intensity of a murmur is not a consistently reliable indication of the severity of the causative lesion. Specific causes include valvular incompetence or stenosis, abnormal vascular or cardiac chamber communications, anemia, fever, and anxiety.
Murmurs, which may be innocent (associated with alterations in blood flow, but not with organic cardiac disease) or pathologic (associated with cardiac disease), are classified by their location, duration, timing within the cardiac cycle, intensity, and character. Murmurs may be systolic (occurring during systole - between S1 and S2) or diastolic (occurring during diastole - between S2 and S1), and are described as continuous or holo- (or pan-), early, mid-, and late systolic or diastolic (Figure 1). The intensity of heart murmurs is graded on a scale of I to VI as described by Ettinger (Table 1). The pitch of the murmur, described as high, low, or mixed frequency, may help to identify the underlying disorder. An important diagnostic clue, especially in the instance of congenital heart disease, is the further characterization of murmurs according to their quality. Regurgitant murmurs are rectangular or plateau-shaped, and ejection murmurs are diamond-shaped or crescendo-decrescendo in nature (Figure 1). A cardiologist's description of a murmur might read: "a grade V, holosystolic, mixed frequency, regurgitant murmur, most audible over the fifth left intercostal space (mitral valve region)."
Table 1. Grading heart murmurs
|
I
|
Soft
|
Murmur barely audible, with minimal radiation
|
|
II
|
Soft
|
Murmur very soft, but definitely audible, radiates more widely than I
|
|
III
|
Mod
|
Murmur easily audible but low in intensity, radiates relatively widely
|
|
IV
|
Mod
|
Murmur moderately intense without precordial thrill, radiates widely
|
|
V
|
Loud
|
Murmur is loud and associated with precordial thrill, heard over entire thorax
|
|
VI
|
Loud
|
Murmur very loud and audible, audible with stethoscope removed from thorax
|
Adapted from Ettinger.
Systolic regurgitant murmurs are associated with mitral and tricuspid insufficiency and ventricular septal defects (Figures 1, 4 and 5). Systolic ejection murmurs suggest pulmonic or aortic stenosis or atrial septal defect (Figure 4). Continuous murmurs are produced by arteriovenous connections (patent ductus arteriosus or arteriovenous fistulae (Figures 1 and 4). Diastolic murmurs, which are uncommonly encountered, are associated with semilunar valvular insufficiency or atrioventricular valvular stenosis (Figure 1). Non-continuous, systolic-diastolic murmurs are most often associated with vegetative endocarditis.
| Figure 4 | 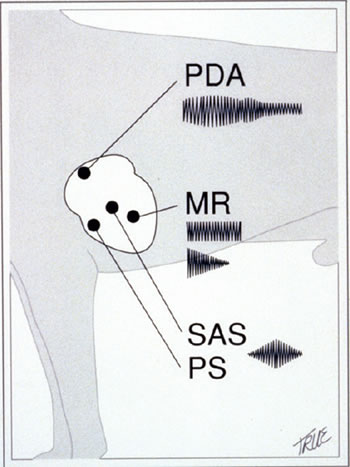
|
|
| |
| Figure 5 | 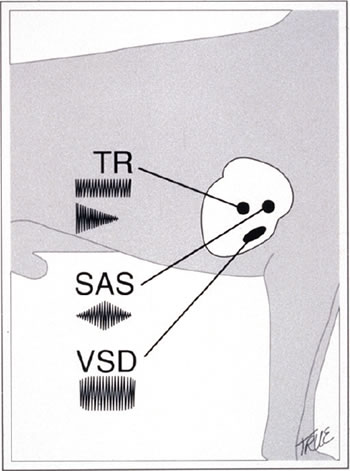
|
|
| |
Innocent murmurs, characterized by low intensity (lower than grade III) and short duration, are relatively common in young dogs (younger than 6–12 months), and must be distinguished from the murmurs of congenital heart disease. These innocent or functional murmurs, due to turbulent flow in the great vessels during ventricular infection, often change in character or disappear when the patient's position is altered. Such murmurs usually do not persist into adulthood. Likewise, the murmurs of anemia (packed-cell volume less than 20%), fever, anxiety, or pregnancy are not associated with structural cardiac disease and have been termed physiologic murmurs.
Split Heart Sounds
Either the first (S1) or second (S2) heart sound may be split, producing two nearly simultaneous sounds, similar in quality to the single sound from which they arose ("lub-lub dub") or "lub dub-dub" for split S1 or S2, respectively). Splitting of the first heart sound is produced by asynchronous closure of the atrioventricular valves. While it is considered to be normal in large-breed dogs, it may be associated with ventricular conduction disturbances, ventricular pacing, or arrhythmias (Figure 1). Splitting of the second heart sound occurs when the semilunar valves close asynchronously (Figure 1). Normally, the aortic valve closes slightly before the pulmonic valve. Splitting of S2 is most frequently associated with delayed closure of the pulmonic valve, as is seen in pulmonary hypertension (usually due to heartworm disease), pulmonic stenosis, or right bundle branch block, or in normal dogs during inspiration. It is occasionally observed with early closure of the aortic valve in states of diminished left ventricular output. Paradoxical splitting of S2 results when significant prolongation of left ventricular conduction and/or ejection time (left bundle branch block, subaortic stenosis, systemic hypertension, or severe left ventricular hypertrophy) delays closure of the aortic valve until after pulmonic valve closure.
Cardiac Gallops
Cardiac gallops or gallop rhythms, consisting of a series of sounds reminiscent of a galloping horse, are composed of S1, S2, and S3 or S4 ("lub dub thud"); the extra sound is of low frequency and may be difficult to hear. Cardiac gallops occur when S3 (protodiastolic gallop), S4 (presystolic gallop), or a combination of S3 and S4 (summation gallop) is abnormally accentuated (Figure 1). S3 gallops are produced when blood rushes into an incompletely emptied ventricle during rapid ventricular filling (e.g., in mitral insufficiency or dilated cardiomyopathy), while S4 gallops result when a noncompliant ventricle (e.g., hypertrophic cardiomyopathy) receives blood during atrial systole. Cardiac gallops are considered to be pathologic in dogs and cats, and are often associated with a poor prognosis.
Systolic Clicks
Systolic clicks are abnormal, usually midsystolic, high-frequency sounds associated with mitral valve prolapse in humans. They are thought to be a preregurgitant phenomenon in dogs or are variably associated with systolic murmurs of mitral regurgitation (Figure 1).
Sounds Associated with Pericardial Disease
Friction rubs, associated with pericarditis and rarely heard in small animals, are "scratchy" biphasic or triphasic sounds audible during portions of both systole and diastole. They occur when inflamed and roughened pericardial and epicardial surfaces contact each other.
A pericardial bump, variable in its number of components and intensity, accompanies early diastolic ventricular filling in the presence of restrictive pericarditis. It occurs when the rapidly filling ventricles are suddenly restricted by the limiting pericardium.
Muffled Heart Sounds
Attenuation of muffling of normal heart sounds may be an important indicator of thoracic disease. Disorders associated with muffled heart sounds include pericardial and pleural effusion, diaphragmatic hernias, thoracic neoplasia, obesity, and hypothyroidism.
Audible Arrhythmias
Certain arrhythmias, such as sinus arrhythmia and atrial fibrillation, are virtually diagnostic upon cardiac auscultation when the femoral pulse is palpated concurrently. Sinus arrhythmia is "regularly irregular" without pulse deficits, and changes in rate are usually associated with respiration. Atrial fibrillation is characterized as being "irregularly irregular," with marked variability in the intensity of S1, variable pulse strength, and frequent pulse deficits. Unifocal ventricular tachycardia is typically regular, and the pulses, although often weak, are palpable and without deficits. Supraventricular (atrial or junctional) tachycardia tends to be very rapid, but is difficult to distinguish from sinus and ventricular tachycardia without electrocardiographic evaluation. Abrupt cessation of a tachyarrhythmia with administration of a vagal maneuver is diagnostic of supraventricular tachycardia. Isolated supraventricular and ventricular ectopic beats produce early, abnormal heart sounds (often only S1 is heard), followed by a pause and typically weak or non-existent pulse. With sinus bradycardia or second- and third-degree heart block, the rate is slow and there is no pulse deficit. Sounds of atrial systole may occasionally be appreciated between the sounds of ventricular systole in high-grade AV block. In the case of first- and second-degree atrioventricular block, S4 (atrial systole) can occasionally be heard.
Diagnostic Approach and Management
The diagnostic approach to the finding of cardiac auscultatory abnormalities varies with the abnormality, the accompanying clinical picture, and the client's wishes. The finding of a supposedly innocent murmur in a healthy pup requires no more than a follow-up examination at the next vaccination appointment. Conversely, the finding of a systolic-diastolic murmur in a dog with fever, joint pain, and dyspnea may require a complete cardiologic and medical workup, blood cultures, and hospitalization.
If the abnormal heart sound(s) cannot be accurately characterized, its exact character can often be determined by obtaining a phonocardiogram (Figure 1). This procedure, although not routinely available in private practice, may be necessary to determine the exact timing or character of a murmur and the type of gallop, or in distinguishing, for example, whether a subtle sound is a gallop, split sound, or systolic click. Phonocardiography is particularly useful in small animal practice where such factors as uncooperative patients, rapid heart rates, and panting or purring decrease the sensitivity and accuracy of cardiac auscultation. Electronic digital stethoscopes, which allow the murmur to be recorded and replayed at half speed, may also be employed in cases in which the character of a murmur or exact nature of an abnormal heart sound is difficult to accurately assess.
Once abnormal sounds have been identified, the goal is to determine the presence, severity, and exact nature of underlying cardiac disease. This is accomplished by performing the following procedures, when indicated: thoracic radiography, electrocardiography, extended electrocardiographic (Holter) monitoring, echocardiography with or without Doppler studies, blood gas analysis, and cardiac catheterization (selective or nonselective) with oximetry, pressure measurement, and angiography. The indications for such procedures and the expected results are explored in greater detail in subsequent chapters.
Patient Monitoring
Depending on the diagnosis, the patient's condition, and the prognosis, a follow-up schedule is established. This timing is variable, but may require no more frequent visits than the yearly vaccination appointment. Patients with more severe afflictions (those with impending heart failure, heart failure, or potentially life-threatening arrhythmias) obviously require more frequent reevaluation. It should be emphasized that if the nature of an abnormal heart sound or the resultant diagnosis is unclear, referral to a specialist with the expertise and specialized equipment to effect a more in-depth examination and evaluation is advisable.