Sharon A. Center, DVM, DACVIM
The feline hepatic lipidosis syndrome (HL) is a potentially lethal intrahepatic cholestatic syndrome observed in over conditioned (obese) cats associated with anorexia and catabolism. This circumstance commonly complicates other liver disorders in the cat and a thorough approach to its management entertains therapeutic maneuvers thought to have benefit in many jaundiced cats. Successful recovery from feline liver disorders improves with early diagnosis and requires a committed effort to provide nutritional and metabolic support. Since cats have a unique propensity for accumulation of lipid vacuoles in their hepatocytes, there has been confusion in some cases where the HL syndrome was diagnosed in an individual having only minor to moderate cell vacuolation (histopathology or cytology). In the HL syndrome > 80% of hepatocytes are involved; in health, only 5% of hepatic weight is attributed to triglyceride. The disorder is best considered a syndrome as it has a multifactorial pathogenesis leading to malnutrition. The old term "idiopathic" associated with this condition is obsolete since in most cases (>85% in the author's clinic) a more primary disease condition can be identified as the underlying problem.
Disorders Associated with Secondary Feline Hepatic Lipidosis Syndrome
|
Other liver disorders: |
Small intestinal diseases: |
|
Cholangiohepatitis |
Eosinophilic enteritis |
|
Choledochitis |
Lymphocytic/plasmacytic enteritis |
|
--extrahepatic bile duct obstruction |
Chronic bowel obstruction |
|
Chronic suppurative hepatitis |
Salmonella enteritis |
|
Portosystemic vascular anomaly |
|
|
Bile duct adenocarcinoma |
Renal disorders |
|
Hepatic lymphosarcoma |
Chronic FUS |
|
Neoplasia (non-hepatic): |
Pyelonephritis |
|
Urinary bladder |
Chronic interstitial nephritis |
|
--transitional cell carcinoma |
Hyperthyroidism |
|
Metastatic carcinoma |
Severe Anemia |
|
Intestinal adenocarcinoma |
Pyometra |
|
Intestinal lymphosarcoma |
Cardiomyopathy |
|
Pancreatitis |
Central neurologic disease |
|
Diabetes mellitus |
|
Confirming the Diagnosis of Hepatic Lipidosis
 Don't be in a hurry to acquire tissue if hepatic lipidosis is a primary consideration.
Don't be in a hurry to acquire tissue if hepatic lipidosis is a primary consideration.
 Use cytology & clinicopathologic features to make a presumptive diagnosis.
Use cytology & clinicopathologic features to make a presumptive diagnosis.
 During the initial few days of therapy / rescue, these animals have high risk for anesthetic / surgical complications.
During the initial few days of therapy / rescue, these animals have high risk for anesthetic / surgical complications.
 We have observed Heinz body hemolysis after: etomidate and diazepam sedation (propylene glycol carrier), and after propofol anesthesia (phenol derivative). Usually, the Heinz body crisis hits about 12-hours after drug administration.
We have observed Heinz body hemolysis after: etomidate and diazepam sedation (propylene glycol carrier), and after propofol anesthesia (phenol derivative). Usually, the Heinz body crisis hits about 12-hours after drug administration.
 Early liver biopsy may lead to death: related with failure to recover from anesthesia or bleeding.
Early liver biopsy may lead to death: related with failure to recover from anesthesia or bleeding.
 A presumptive diagnosis of HL is made on the basis of: Signalment, physical examination, clinicopathologic data, and abdominal ultrasound. This justifies hepatic needle aspiration for cytology. However, this procedure is only done after vitamin K1 response. Liver biopsy is really not necessary to diagnose HL, however it is necessary to diagnose cholangitis / cholangiohepatitis (suppurative or non-suppurative) and other liver disorders. Make sure that > 80% of hepatocytes are vacuolated on aspiration cytology and that hepatocytes were sampled, not just omental / falciform fat.
A presumptive diagnosis of HL is made on the basis of: Signalment, physical examination, clinicopathologic data, and abdominal ultrasound. This justifies hepatic needle aspiration for cytology. However, this procedure is only done after vitamin K1 response. Liver biopsy is really not necessary to diagnose HL, however it is necessary to diagnose cholangitis / cholangiohepatitis (suppurative or non-suppurative) and other liver disorders. Make sure that > 80% of hepatocytes are vacuolated on aspiration cytology and that hepatocytes were sampled, not just omental / falciform fat.
 When to Pursue a Liver Biopsy? If poor response: feeding attempts fail, bilirubin does not decline, clinical illness persists at a severe level after 7-10 days of critical supportive care.
When to Pursue a Liver Biopsy? If poor response: feeding attempts fail, bilirubin does not decline, clinical illness persists at a severe level after 7-10 days of critical supportive care.
Fluid & Treatments Routinely Used in Rescuing Cats with Hepatic Lipidosis
 Fluids: Avoid lactate containing and dextrose supplemented fluids. High lactate associated with HL. Dextrose supplementation may thwart adaptation to fatty acid oxidation; carbohydrates poorly handled in stressed cats.
Fluids: Avoid lactate containing and dextrose supplemented fluids. High lactate associated with HL. Dextrose supplementation may thwart adaptation to fatty acid oxidation; carbohydrates poorly handled in stressed cats.
 KCl Supplementation: according to the conventional sliding scale. Do not exceed 0.5 mEq/kg/hr KCl. If concurrently supplementing K phosphate, reduce KCl dose by amount of K in K phosphate.
KCl Supplementation: according to the conventional sliding scale. Do not exceed 0.5 mEq/kg/hr KCl. If concurrently supplementing K phosphate, reduce KCl dose by amount of K in K phosphate.
 Potassium Phosphate Supplementation: Phosphate concentrations decline after initial feeding (refeeding phenomenon). Initial dose of 0.01 to 0.03 mmol/kg/hr. Usually use the high dose rate, even if initial phosphate is not low, upon refeeding hypophosphatemia frequently develops. Monitor serum phosphate concentrations every 3 to 6 hours (during and immediately after discontinued supplementation). Discontinue phosphate infusion when serum phosphorus > 2 mg/dl. Complications: Too much phosphate can result in hypocalcemia and soft tissue calcium-phosphate deposition. Calcium-phosphorus product > 58 mg/dl = mineralization. Iatrogenic hyperkalemia: failure to appropriately reduce KCl infusion rate. Parenteral requirements resolve once alimentation established.
Potassium Phosphate Supplementation: Phosphate concentrations decline after initial feeding (refeeding phenomenon). Initial dose of 0.01 to 0.03 mmol/kg/hr. Usually use the high dose rate, even if initial phosphate is not low, upon refeeding hypophosphatemia frequently develops. Monitor serum phosphate concentrations every 3 to 6 hours (during and immediately after discontinued supplementation). Discontinue phosphate infusion when serum phosphorus > 2 mg/dl. Complications: Too much phosphate can result in hypocalcemia and soft tissue calcium-phosphate deposition. Calcium-phosphorus product > 58 mg/dl = mineralization. Iatrogenic hyperkalemia: failure to appropriately reduce KCl infusion rate. Parenteral requirements resolve once alimentation established.
 Vitamin K: 0.5 to 1.5 mg/kg PO at 12 hour intervals parenterally, not IV and not PO, 2-3 doses only.
Vitamin K: 0.5 to 1.5 mg/kg PO at 12 hour intervals parenterally, not IV and not PO, 2-3 doses only.
 Vitamin E: 10 IU/ kg PO per day until convinced of recovery.
Vitamin E: 10 IU/ kg PO per day until convinced of recovery.
 Water Soluble Vitamins: 1-2 ml B Soluble vitamins per liter, keep covered from light.
Water Soluble Vitamins: 1-2 ml B Soluble vitamins per liter, keep covered from light.
 Thiamine (B1): 100 mg orally, use B-soluble vitamins in fluids not SQ or IM injection - collapse (rare).
Thiamine (B1): 100 mg orally, use B-soluble vitamins in fluids not SQ or IM injection - collapse (rare).
 B12-Cobalamin: B-soluble vitamin supplementation in fluids and commercially available critical care diets (commercial pet foods are supplemented with stable, pharmaceutical grade vitamin B12) can provide therapeutic B12 for many patients. However, those with severe inflammatory bowel disease or malabsorption due to infiltrative bowel disease (including lymphoma) may require parental "loading" and protracted therapy with parenterally administered B12 (1 mg IM). Frequency of dose administration is determined based on sequential plasma B12 concentrations (5-7 day intervals to once monthly have been determined in individual cats). B12 insufficiency may augment development of hepatic lipidosis.
B12-Cobalamin: B-soluble vitamin supplementation in fluids and commercially available critical care diets (commercial pet foods are supplemented with stable, pharmaceutical grade vitamin B12) can provide therapeutic B12 for many patients. However, those with severe inflammatory bowel disease or malabsorption due to infiltrative bowel disease (including lymphoma) may require parental "loading" and protracted therapy with parenterally administered B12 (1 mg IM). Frequency of dose administration is determined based on sequential plasma B12 concentrations (5-7 day intervals to once monthly have been determined in individual cats). B12 insufficiency may augment development of hepatic lipidosis.
 l-Carnitine: 250 mg PO / day has been used as a routine supplement in the author's hospital for the theoretical reason of promoting fatty acid oxidation, increasing loss of CN-ester fatty acids in urine, and retention of lean body mass. Metabolic response to l-CN has recently been proven in obese healthy cats undergoing weight loss. Synthesis of l-carnitine may be enhanced by SAMe supplementation.
l-Carnitine: 250 mg PO / day has been used as a routine supplement in the author's hospital for the theoretical reason of promoting fatty acid oxidation, increasing loss of CN-ester fatty acids in urine, and retention of lean body mass. Metabolic response to l-CN has recently been proven in obese healthy cats undergoing weight loss. Synthesis of l-carnitine may be enhanced by SAMe supplementation.
 GSH donors: Markedly low hepatic GSH has been demonstrated in liver tissue from cats with HL. May promote RBC hemolysis not attributable to electrolyte aberrations (severe hypophosphatemia), and may be associated with RBC Heinz bodies and adverse response to oxidative drugs (e.g., too much vitamin K, propofol anesthesia, injectable diazepam or etomidate contain propylene glycol).
GSH donors: Markedly low hepatic GSH has been demonstrated in liver tissue from cats with HL. May promote RBC hemolysis not attributable to electrolyte aberrations (severe hypophosphatemia), and may be associated with RBC Heinz bodies and adverse response to oxidative drugs (e.g., too much vitamin K, propofol anesthesia, injectable diazepam or etomidate contain propylene glycol).
 N-acetylcysteine: 140 mg/kg IV, then 70 mg/kg IV at 12 hour intervals. Dilute 10% NAC (Mucomyst®) with saline 1: 4, administer IV using a 0.25 micron filter.
N-acetylcysteine: 140 mg/kg IV, then 70 mg/kg IV at 12 hour intervals. Dilute 10% NAC (Mucomyst®) with saline 1: 4, administer IV using a 0.25 micron filter.
 s-Adenosylmethionine (SAMe; Denosyl-SD4): use source providing S'S stereoisomer = biologically active form only. 20 mg/kg PO BID. Follow NAC as PO thiol (GSH) donor. Since SAMe is given with food in the HL cat which is on continuous nutritional support and since the presence of food reduces SAMe bioavailability, we have empirically increased the total dose by BID administration.
s-Adenosylmethionine (SAMe; Denosyl-SD4): use source providing S'S stereoisomer = biologically active form only. 20 mg/kg PO BID. Follow NAC as PO thiol (GSH) donor. Since SAMe is given with food in the HL cat which is on continuous nutritional support and since the presence of food reduces SAMe bioavailability, we have empirically increased the total dose by BID administration.
Contents of a fortified B-vitamin complex used in crystalloid fluids in cats with FHL.
|
Thiamine hydrochloride (Vitamin B1): |
50 mg |
|
Riboflavin 5' Phosphate sodium (Vitamin B2): |
2.0-2.5 mg |
|
Niacinamide (Vitamin B3): |
50-100 mg |
|
d-panthenol (Vitamin B5): |
5-10 mg |
|
Pyridoxine HCl (Vitamin B6): |
2-5 mg |
|
Cyanocobalamin (Vitamin B12):
(Low B12 values necessitate additional supplementation in deficient cats, IM) |
variable 0.4 to 50 mcg |
|
Benzyl alcohol (preservative): |
1.5% (no adverse consequences noted in FHL cats) |
Nutritional Support: Essential Cornerstone of Therapy for Jaundiced Cats
 Initial Feeding: Use oral feeding or nasogastric (NG) tube. Avoid food aversion response, do not anesthetize for feeding tube insertion until electrolytes, hydration, and vitamin K supplementation have been established (usually 48 to 72 hours). Initial feeding best accomplished using an NG tube. stop oral feeding if salivation, nausea or struggling to get away from the food. After a few days of rehydration, corrected electrolytes, improved vitality, response to vitamin K, you have an optimal situation for placing an E-tube.
Initial Feeding: Use oral feeding or nasogastric (NG) tube. Avoid food aversion response, do not anesthetize for feeding tube insertion until electrolytes, hydration, and vitamin K supplementation have been established (usually 48 to 72 hours). Initial feeding best accomplished using an NG tube. stop oral feeding if salivation, nausea or struggling to get away from the food. After a few days of rehydration, corrected electrolytes, improved vitality, response to vitamin K, you have an optimal situation for placing an E-tube.
 Feeding Tubes: Nasogastric / nasoesophageal tube initially, followed by placement of an E-tube (preferred).
Feeding Tubes: Nasogastric / nasoesophageal tube initially, followed by placement of an E-tube (preferred).
 General Tips for Feeding Tube Care: Maintenance of tube hygiene is essential. Flush with warm water after each feeding with enough volume to cleanse the tube yet not fill stomach. Avoid putting pill form of medications that can cause concretions (some ground up medications congeal in liquid form) into narrow feeding tubes; may cause tube occlusion.
General Tips for Feeding Tube Care: Maintenance of tube hygiene is essential. Flush with warm water after each feeding with enough volume to cleanse the tube yet not fill stomach. Avoid putting pill form of medications that can cause concretions (some ground up medications congeal in liquid form) into narrow feeding tubes; may cause tube occlusion.
 If G-Tube: Aspirate tube before feeding to evaluate gastric emptying: > 10 ml = gastric hypokinesia that may reflect either electrolyte derangements or pain derived from gastrostomy tube (site infection, leakage, insertion causing mechanical restriction of gastric motility.
If G-Tube: Aspirate tube before feeding to evaluate gastric emptying: > 10 ml = gastric hypokinesia that may reflect either electrolyte derangements or pain derived from gastrostomy tube (site infection, leakage, insertion causing mechanical restriction of gastric motility.
 Check Ostomy Site: 1-2x daily for the first 10 days. Perform cytology on ANY discharge. Avoid infection as this complicates recovery. Visually inspect the anchoring sutures.
Check Ostomy Site: 1-2x daily for the first 10 days. Perform cytology on ANY discharge. Avoid infection as this complicates recovery. Visually inspect the anchoring sutures.
 If Persistent Vomiting: Check electrolytes:rule out severe hypokalemia or hypophosphatemia; ensure that feeding tube is not causing gastric outflow obstruction; radiographic contrast injection (Renografin) or by use of ultrasound (US). Provide some modest exercise: may stimulate enteric motility
If Persistent Vomiting: Check electrolytes:rule out severe hypokalemia or hypophosphatemia; ensure that feeding tube is not causing gastric outflow obstruction; radiographic contrast injection (Renografin) or by use of ultrasound (US). Provide some modest exercise: may stimulate enteric motility
 Antiemetics
Antiemetics
 Metoclopramide:
Metoclopramide:
 0.01-0.02 mg/kg/hr IV constant rate infusion / 24 hours
0.01-0.02 mg/kg/hr IV constant rate infusion / 24 hours
 0.2-0.4 mg/kg SQ 20 min. before meal
0.2-0.4 mg/kg SQ 20 min. before meal
 Ondansetron:
Ondansetron:
 5 HT3 receptor antagonist (expensive, oral only)
5 HT3 receptor antagonist (expensive, oral only)
 0.1-1.0 mg/kg q 12-24 hrs
0.1-1.0 mg/kg q 12-24 hrs
 Trickle Feed: Slow rate / 24 hours continuous feeding of a liquefied diet through an infusion pump. Running feeding line through a warm water bath (bowl of warm water) may assist food flow through small tube lumen. Re-new food q 4-6 hours to avoid bacterial contamination.
Trickle Feed: Slow rate / 24 hours continuous feeding of a liquefied diet through an infusion pump. Running feeding line through a warm water bath (bowl of warm water) may assist food flow through small tube lumen. Re-new food q 4-6 hours to avoid bacterial contamination.
 IF Still Persistent Vomiting: Double check tube for problems (contrast radiography, US)
IF Still Persistent Vomiting: Double check tube for problems (contrast radiography, US)
 If Tube occlusion: Problem typically restricted to G-tubes, use solutions that can digest food: Coca Cola, papaya juice, or pancreatic enzymes. Let dwell 20 to 40 minutes; then flush well with lukewarm water. Do not attempt to clear tube with a solid stilette: may penetrate tube or patient. Radiographically re-evaluate tube patency/position.
If Tube occlusion: Problem typically restricted to G-tubes, use solutions that can digest food: Coca Cola, papaya juice, or pancreatic enzymes. Let dwell 20 to 40 minutes; then flush well with lukewarm water. Do not attempt to clear tube with a solid stilette: may penetrate tube or patient. Radiographically re-evaluate tube patency/position.
 Diet to Feed: Do not restrict protein unless signs of hepatic encephalopathy. Feed maximum calorie balanced feline foods.
Diet to Feed: Do not restrict protein unless signs of hepatic encephalopathy. Feed maximum calorie balanced feline foods.
 How Much to Feed: 60-90 kcal/kg body wt per day. Start with a liquid diet through NG tube. Initially administer 5 ml of lukewarm water at 2-hr intervals 2-to 3-times to determine the likelihood of emesis & gastric atony. Food is progressively introduced over a 2 to 4 day interval to achieve intake of between 250 to 400 kcal per day for the average sized cat. If G-tube used, initial feeding is delayed for 24-36 hours after tube insertion to allow return of gastric motility and to permit formation of an initial wound seal around the insertion site. Feeding through an E-tube may be initiated after full recovery from the anesthetic restraint.
How Much to Feed: 60-90 kcal/kg body wt per day. Start with a liquid diet through NG tube. Initially administer 5 ml of lukewarm water at 2-hr intervals 2-to 3-times to determine the likelihood of emesis & gastric atony. Food is progressively introduced over a 2 to 4 day interval to achieve intake of between 250 to 400 kcal per day for the average sized cat. If G-tube used, initial feeding is delayed for 24-36 hours after tube insertion to allow return of gastric motility and to permit formation of an initial wound seal around the insertion site. Feeding through an E-tube may be initiated after full recovery from the anesthetic restraint.
 Avoid reliance on appetite modifiers Diazepam, Oxazepam, Cyproheptadine: do not ensure adequate nutritional intake. Diazepam and Oxazepam are benzodiazepines which are considered hepatoencephalogenic toxins. These require hepatic biotransformation and conjugation for elimination (the HL cat is presumably deficient in these processes).
Avoid reliance on appetite modifiers Diazepam, Oxazepam, Cyproheptadine: do not ensure adequate nutritional intake. Diazepam and Oxazepam are benzodiazepines which are considered hepatoencephalogenic toxins. These require hepatic biotransformation and conjugation for elimination (the HL cat is presumably deficient in these processes).
 If Neck Ventroflexion: Consider electrolyte or thiamine insufficiency. In these cats be sure to monitor electrolytes (K, P, Mg) and to correct any insufficiencies. Cats with HL may waste potassium in urine. Those with hypokalemia that is difficult to correct may be magnesium deficient. Since there is no single test that rules out thiamine deficiency as a cause of neck ventroflexion (and also neurologic signs confused with hepatic encephalopathy) you should administer thiamine: 100 mg in fluids (B-soluble vitamins given slowly with crystalloid fluids) and supplement with 100 mg via enteric route daily. Parenteral administration of injectable thiamine (intramuscular thiamine HCl may rarely cause vasovagal collapse and neuromuscular paralysis; mechanism unknown).
If Neck Ventroflexion: Consider electrolyte or thiamine insufficiency. In these cats be sure to monitor electrolytes (K, P, Mg) and to correct any insufficiencies. Cats with HL may waste potassium in urine. Those with hypokalemia that is difficult to correct may be magnesium deficient. Since there is no single test that rules out thiamine deficiency as a cause of neck ventroflexion (and also neurologic signs confused with hepatic encephalopathy) you should administer thiamine: 100 mg in fluids (B-soluble vitamins given slowly with crystalloid fluids) and supplement with 100 mg via enteric route daily. Parenteral administration of injectable thiamine (intramuscular thiamine HCl may rarely cause vasovagal collapse and neuromuscular paralysis; mechanism unknown).
Predicting Recovery from Hepatic Lipidosis
Cats making a successful clinical recovery from HL demonstrate a gradual reduction in serum enzyme activities and total bilirubin concentrations over time. Generally, within 10 days the total bilirubin concentration declines by > 50% while serum enzyme activity may remain near values documented at the time of case admission. Cats with severe HL making a successful recovery required 10 days (median) of hospitalization; those that died did so by day 7 (median). Surviving cats my require up to 21 days of hospital care, depending on the owner's nursing skill and desire to participate in the cat's care. Treatment with l-carnitine and the regimen outlined above has not reduced the length of hospitalization of cats in our clinic. However, a chance of recovery > 85% can be estimated in our hospital if an individual cat survives the initial 96 hours.
| 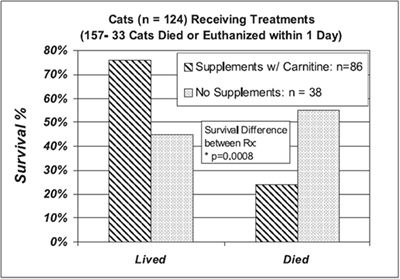
Survival in cats with severe hepatic lipidosis receiving balanced nutritional support and supplements described in these notes or without supplements |
|
| |