Department of Clinical Sciences of Companion Animals, Faculty of Veterinary Medicine, Utrecht University
The Netherlands
1. General considerations
Intervertebral disc disease (IVDD) is a frequent neurologic problem affecting dogs and occurs rarely in cats. Disc diseases in canines occur in the cervical, thoracic, lumbar and lumbosacral region. The end of the spinal cord in dogs lies inside lumbar vertebra L6. Cervical and thoracolumbar disc disease affect the spinal cord whereas lumbosacral disc disease affects the cauda equina. The intervertebral disc consists of the ring-like, fibrous, collagen-rich annulus fibrosus and the central, gelatinous, water-rich nucleus pulposis. Degeneration of discs is associated with decreased water content and two types are distinguished: 1) Hansen type I degeneration: chondroid degeneration with extrusion of nucleus material through a ruptured dorsal annulus fibrosus and the dorsal longitudinal ligament into the vertebral canal, and 2) Hansen type II degeneration: fibroid degeneration with bulging or protrusion of the partially ruptured and thickened annulus fibrosus.
When the intervertebral disc ruptures and herniates, it causes damage to the nervous system which initially results in pain. The pain suffered with disc disease arises from several sources: 1) discogenic pain (stretching or ruptures in the annulus fibrosus), 2) meningeal pain (mechanical contact or mass effect of extruded disc material on the meninges [dura mater] and/or foreign body inflammatory response to nucleus pulposis material in vertebral canal), 3) radicular pain (compression or entrapment of nerve roots, 'root signature'). The spinal cord itself has no sensory nerve fibers.
Injury to the spinal cord may ultimately lead to neurological deficits and with increasing pressure and/or longer duration the extent of deficits may be more prominent and less reversible. An extradural mass in the spinal canal will exert its effect on the spinal cord from the periphery to the center. The neuroanatomic background explains the classical stepwise development of deficits: ataxia (loss of coordination, loss of proprioception)>>paresis (muscle weakness)>>paralysis (loss of voluntary motor function)>>loss of deep pain sensation. The proprioceptive (position sense) nerve fibers are the largest, and most susceptible to compressive forces and lie superficially in the dorsal funiculus. In contrast, the small deep pain nerve fibers that are most resistant to pressure lie in deeply positioned spinothalamic tracts. This explains why loss of deep pain perception is such a severe clinical sign. Based on the neuroanatomy a scale of neurological deficits is possible which will be used in the description of patients with cervical and thoracolumbar disc disease.
| Figure 1. | 
American Cocker Spaniel with cervical pain. |
|
| |
2. Neurological grading in canine intervertebral disc disease:
 Grade 0: normal.
Grade 0: normal.
 Grade 1: cervical or thoracolumbar pain, hyperaesthesia.
Grade 1: cervical or thoracolumbar pain, hyperaesthesia.
 Grade 2: paresis (muscle weakness) with decreased proprioception, ambulatory (able to walk).
Grade 2: paresis (muscle weakness) with decreased proprioception, ambulatory (able to walk).
 Grade 3: severe paresis with absent proprioception, not ambulatory (not able to walk).
Grade 3: severe paresis with absent proprioception, not ambulatory (not able to walk).
 Grade 4: paralysis (not able to stand or walk), decreased or no bladder control, conscious deep pain perception present.
Grade 4: paralysis (not able to stand or walk), decreased or no bladder control, conscious deep pain perception present.
 Grade 5: paralysis, urinary and fecal incontinence, no deep conscious pain perception.
Grade 5: paralysis, urinary and fecal incontinence, no deep conscious pain perception.
Neurological grading in canine IVDD is valuable to follow the progression of neurological deficits in time (improvement or worsening), to choose the mode of therapy, for prognosis, and for assessment of outcome after medical or surgical treatment.
3. Cervical disc disease
Cervical disc disease is a frequent disorder in dogs. Small breeds, particularly those with chondrodystrophic characteristics, are commonly affected, but it can occur in any dog. Dachshunds, Beagles, Poodles, Spaniels, Shih Tzus, Pekingese, and Chihuahuas are most often affected. Most small dogs are older than 2 years with a mean of 6-7 years. Disc disease is rare in dogs less than one year. There is no sex predilection.
Doberman and other large breeds (e.g., Rottweiler) suffer from cervical disc disease (Hansen type II disc degeneration) as part of the syndrome of caudal cervical spondylomyelopathy (CCSM, wobbler syndrome) which is not the topic of this abstract.
Clinical Signs
The predominant clinical sign is severe neck pain which may be acute or chronic. Often pain is unremitting and unresponsive to medication. Dogs may scream spontaneously or upon approach. Affected dogs may be reluctant to eat unless the food is raised from the floor. The dog often shows low head carriage and hunched back (kyphosis) (Figure 1) leading to misdiagnosis of the pain to the middle back region. Cervical pain is often very easily elicited when the spine or muscles of the neck are palpated where tension and pain are evident. In acute cervical pain it is not necessary to flex or extend the neck. In dogs with chronic pain or in the larger breeds like the Doberman with type II disc disease cervical pain may not be that prominent and flexion, extension, and rotation are necessary to localize the pain.
Neurological deficits in cervical disc disease are usually less frequent than in thoracolumbar disc disease; this is explained by the relative wide spinal canal for the spinal cord in the cervical area compared with the thoracolumbar area. Extradural space-occupying lesions, like disc extrusions, will affect the spinal cord more in the thoracolumbar area than in the cervical area. Not seldom a huge disc extrusions is seen in cervical disc disease that obliterates the vertebral canal for 50% or more while the dog is still ambulatory; whereas a comparable obliteration in the thoracolumbar spine results in paraplegia of the pelvic limbs.
Neurological deficits related to cervical spinal cord compression may be seen: paresis or lameness in a thoracic limb are most frequent. However, hemiparesis, tetraparesis, and tetraparalysis may also occur. Nerve root signature (pain apparent on palpation or traction of the limb) is another frequent finding. Nerve root signature is more often a feature of caudal disc involvement (C5/C6, C6/C7, C7/T1). Decreased or absence of deep pain sensation is an uncommon finding in cervical disc disease.
Disc herniation follows degeneration of the disc. Most occurrences are Hansen Type I extrusions, Hansen type II protrusions do occur, generally in larger breed of dogs such as the Dobermann. The C2/C3 disc is most frequently affected, with the incidence decreasing caudally. The C6/C7 disc is rarely affected, with the exception of Dobermans and other large breeds as part of CCSM. The C7/T1 disc herniates occasionally.
Diagnosis
The diagnosis is based on clinical signs and confirmation by radiographic demonstration of narrowing (collapse) of the intervertebral disc space and dorsal displacement of mineralized disc material (Figure 2). In chondrodystrophic breeds often a mineralized nucleus pulposus is seen, situated in the center of the disc space without narrowing of the space (discopathy). These sites are usually not the cause of the cervical pain. Instead one should look for the disc space that is narrowed as the cause of the cervical pain. Only in cases with a single, isolated, calcified mush-room extrusion (usually C2/C3 or C3/C4) the survey radiographs may be sufficient informative for surgical therapy. In most cases cervical myelography (injection of contrast medium in the cisterna magna) is required to confirm the diagnosis and to localize the extent of compression especially in cases with multiple discs that may potentially be involved. Lateral (Figure 3), ventrodorsal, and oblique views are necessary. Oblique views may reveal the offending disc even as lateral and ventrodorsal projections of the myelogram are normal.
| Figure 2. | 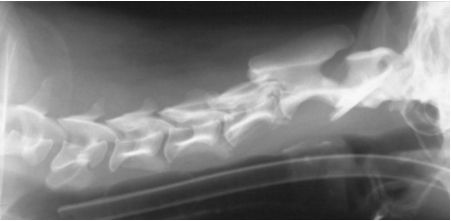
C2-C3: collapsed intervertebral disc space with extruded calcification: HNP type I |
|
| |
| Figure 3. | 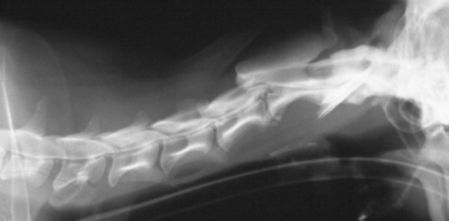
Cervical myelogram: ventral spinal cord compression by HNP type I at C2-C3 |
|
| |
In specialized veterinary institutions with (spiral) computed tomography (CT) and/or magnetic resonance imaging (MRI), these imaging techniques replace myelography. When available, especially MRI has become the technique of choice for diagnosis of intervertebral disc disease in the dog and cat. MRI allows for sagittal scanning of the whole spine; discs and spinal cord can be assessed in the same image. On T2-weighted MR images the nucleus pulposis of a normal disc gives a white signal (high water content). Therefore, a T2-weighted sagittal view of the spine quickly reveals the degenerated discs (decreased water content) that give a decreased or absence of the white nucleus pulposis signal ('black disc'). On transverse MR images at the level of the black disc the extent and lateralization of the disc extrusion can be assessed. A major advantage of MRI is also that in neurologically deficient cases the spinal cord can be assessed and indications for ischemic myelopathy may be evident from MR images.
Treatment
Treatment options may be nonsurgical or surgical.
Nonsurgical treatment. Cage rest and anti-inflammatory medications are installed. It is appropriate to try this treatment with patients with cervical pain and no severe neurological deficits (grade 1 or 2) since many patients with cervical disc disease respond well to medical treatment. NSAIDS or corticosteroids may be used, provided that strict cage rest is installed. NSAIDs and corticosteroids should not be combined. Worsening of the neurological status with medical treatment seen in thoracolumbar disc disease is rare in cervical disc disease. Progression of cervical pain or lack of response to nonsurgical treatment in 1 or 2 weeks indicates treatment failure. A dog that responds well to treatment should be kept rested for 2 to 4 weeks. Recurrence of clinical signs after nonsurgical treatment occurs in 40% of patients.
Surgical treatment. Indications for surgical treatment includes failure of nonsurgical treatment, marked or progressive worsening of neurological deficits, and severe unremitting pain. Ventral fenestration or ventral decompression (ventral slot) are the most frequently performed procedures. Rare cases may require dorsal laminectomy. Indications for ventral decompression are the presence of neurological deficits and myelographic evidence of spinal cord compression. Ventral fenestration will not be sufficient in case there is spinal cord compression. The current opinion is that ventral decompression is the optimal treatment. Fenestration alone should be reserved for those cases with unremitting pain, failure to non-surgical treatment and when myelography is unable to show spinal cord compression at the affected disc site. The dog is positioned in dorsal recumbent position and care is taken not to overextend the head and cranial cervical area. The caudal cervical area is elevated with supportive bags. Accurate identification of the intervertebral discs in the ventral approach is important and is done by palpation of the large transverse processes of C6 that are directed ventrally and the ventral processes in the midline; the intervertebral disc lies immediately caudal to the ventral process. There is no intervertebral disc between C1/C2. The ventral slotting is performed with powered instruments (electrical or air pressure). Burring is progressed until the inner cortical lamina is thinned out. Rongeurs are used to enlarge the opening. Removal of extruded nucleus pulposis material from the vertebral canal provides the most rapid resolution of clinical signs. Fenestration is a useful prophylactic procedure and can be performed on the other cervical discs at the time of ventral slotting.
Postoperative care consists of restricted exercise for 4 weeks and NSAIDs for 1 week. Dogs with severe neurological deficits benefit from physiotherapy or aquatic therapy once the pain has subsided. In cases that are not recumbent, great care to bedding and hygiene is required to prevent decubitus or urinary dermatitis. The prognosis for dogs with cervical disc disease is generally good.
4. Thoracolumbar disc disease
Thoracolumbar disc disease is a common condition that predominantly affects chondrodystrophic breeds (e.g., Dachshund). Peak incidence is around 6-7 years of age. Nonchondrodystrophic breeds (e.g., German shepherd) are less frequently affected. Hansen type I disc disease is seen mainly in chondrodystrophic dogs, whereas Hansen type II is more typical for non-chondrodystrophic breeds. Over 50% of all thoracolumbar disc lesions occur at the T12/T13 and T13/L1 disc and over 75% occur between T11/T12 and L1/L2. Lumbosacral disc disease, a cauda equina disease at L6/L7 or L7/S1, occurs frequently in large breed dogs (e.g., Shepherd dogs) and is associated with Hansen type II disc disease, vertebral instability and spinal stenosis and the complex is called degenerative lumbosacral stenosis but will not be discussed further in this abstract.
The pain resulting from thoracolumbar disease is usually less dramatic than that associated with cervical disc disease. The dog may show kyphosis and reluctance to run or jump, and discomfort when picked up or when palpated in the thoracolumbar region. Pain alone may be misinterpreted as being of abdominal origin. Neurological deficits are more prominent in thoracolumbar disc disease than in cervical disc disease and may range from mild posterior ataxia and paresis to complete posterior paralysis and paraplegia (Figure 4), bladder and fecal incontinence, and depressed or absent deep pain sensation in the pelvic limbs. The withdrawal reflex (spinal reflex) should not be mistakenly interpreted as conscious (cerebral) sensation of deep pain applied to the toes. Spinal hyperreflexia in the pelvic limbs is common due to loss of central inhibition on spinal reflexes. The forelimbs are not affected by thoracolumbar disc disease and should be neurologically intact. The neurological deficits are caused by extradural compression and spinal cord injury and the deficits become more severe with greater and longer spinal cord compression. In addition to the actual mass effect, the rate at which spinal cord injury occurs is also important. If it is rapid, like in a explosive rupture of the disc, the spinal cord cannot compensate and more severe neurological deficits occur. In these cases, progressive ischemic myelomalacia (rather than the mass of extradural disc material found during surgery) may be the main cause of the severe neurological deficits. Most of these dogs show grade 4 or 5 deficits. The clinician should be suspicious when this problem arises; in these cases there is progressive loss of pelvic limb reflexes, the level of panniculus cut-off moves cranially and paralyzed dogs become depressed. The prognosis of these dogs is poor.
| Figure 4. | 
Dachshund with posterior paralysis. |
|
| |
Diagnosis
Survey radiographs may give a tentative diagnosis of thoracolumbar disc disease but should never be used as the sole means of confirming the diagnosis when decompressive surgery is planned. Disc space narrowing and radio-opacity of the intervertebral foramen are the most common findings. However, be aware that the thoracic intervertebral disc spaces are normally more narrow than the lumbar disc spaces. In cats, disc disease may occur in the lower lumbar region (L5/L6 and L6/L7) and calcified disc material may be seen in the spinal canal. Myelography is required for confirmation of diagnosis (Figure 5). In case the cervical myelogram stops cranial to the disc lesion because of spinal cord swelling (especially in acute cases) lumbar myelography (injection of contrast medium between L4/L5) may be performed. Lateral and ventral radiographs should be taken. Oblique views are usually required to identify whether the compressive lesion is situated more on the left or the right side which determines the side for the hemilaminectomy. In institutions where CT or MRI is available these techniques replace myelography (see cervical disc disease).
| Figure 5 -. Hansen type 1 lesion at L1-2 - myelogram | 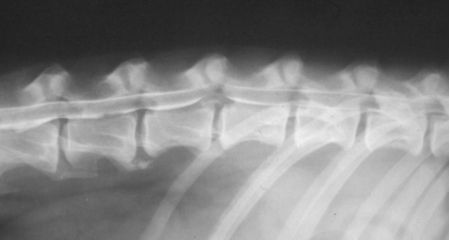
Thoracolumbar myelogram: HNP type I at L1-L2 with ventral spinal cord compression. |
|
| |
Treatment
Treatment options may be nonsurgical or surgical.
Nonsurgical treatment. Strict cage rest is the most important consideration in nonsurgical treatment of thoracolumbar disc disease. Judicious use of anti-inflammatory medication (NSAIDs or corticosteroids) may be helpful. The animal should rest in a confined space (bench) for 2-4 weeks and is only allowed outside the cage for urination and defecation. Animals that do not rest, especially during treatment with NSAIDs, have a great risk of (sudden) deterioration of neurological status with worsening of the prognosis. Overall recovery in dogs with grade 1-3 deficits is 80% to 90%. For paraplegic dogs with grade 4 or 5 deficits non-surgical treatment is rarely the treatment of choice because of the low response rate, high rate of recurrence, neurological worsening during treatment, and development of complications. In dogs with grade 5 neurological deficits the duration of absence of conscious deep pain sensation is an important prognostic parameter. Dogs with grade 5 neurological deficits should be regarded as emergencies and require surgery within 24-48 hours. When grade 5 neurological deficits persist beyond 3 days the result of any treatment (surgical or nonsurgical) becomes minimal.
Surgical treatment. Dorsal right-sided or left-sided hemilaminectomy is the most common surgical treatment for thoracolumbar disc disease (Figure 6). Dorsal laminectomy is not recommended in the thoracolumbar area because it causes considerable biomechanical instability and may lead to neurological worsening. Indications for hemilaminectomy are grade 2 or 3 lesions unresponsive to medical therapy, grade 4 and 5 lesions less than 48 hours duration and myelographic evidence of significant spinal cord compression. The dog is positioned in a ventral recumbent position and supported with bags. Accurate identification of the affected disc is by palpation of the last rib-vertebral body joint and the transverse process of L1. There are frequent anatomical variations in the T13/L1 junction and therefore the survey radiographs (besides the CT or MR images) are required in the operating room to relate anatomic findings during the approach with radiographic findings. Hemilaminectomy is performed using powered instruments and rongeurs. It is performed on the side of the disc herniation which is determined by the myelogram. Fenestration of the affected disc and prophylactic fenestration may be performed of the disc on either side. Fenestration of all high risk discs (T11/T12-L2/L3) requires extensive dissection and is not advised. Burring is progressed until the inner cortical lamina is thinned out. Rongeurs are used to enlarge the opening. Extruded disc material is usually situated lateral and ventral of the spinal cord and frequently entraps the exiting nerve root at the intervertebral foramen. The disc material is removed by the combination of gentle suction, flushing with saline solution and the use of a thin ball-tipped probe to scoop out material from beneath the spinal cord. For closure of the laminar defect an autogenous fat transplant is used to prevent dural adhesions.
| Figure 6. | 
Hemilaminectomy, right side at L1-L2: extruded disc material (grey) |
|
| |
The most important consideration in the postoperative care after hemilaminectomy is to ensure that the bladder is regularly emptied. Urinary retention is the most common postoperative problem in thoracolumbar disc disease. Great care should be given to bedding and hygiene and paraplegic dogs should be bathed at least once a day to prevent decubitus which complicates the recovery. The dogs should be daily examined for pressure points (ischiadic tuberosities) and the perineum should kept clean at any time.
The prognosis for functional recovery is good for dogs with grade 1, 2, and 3 lesions irrespective of the treatment choice. Dogs with grade 4 lesions have better prognosis after surgical treatment than after nonsurgical treatment. In dogs with grade 5 lesions that are treated within 24-48 hours of onset the animal has a chance of making a functional recovery.
References
1. Wheeler SJ, SharpNJH. Small Animal Spinal Disorders. Diagnosis and Surgery. Mosby-Wolfe, London, 1994.
2. Jeffery ND. Handbook of Small Animal Spinal Surgery. WB Saunders, Philadelphia, 1995.