Simon J. Wheeler, BVSc, PhD, DECVN, Dipl Mgmt, FRCVS (Veterinary Neurology)
In this lecture, advances in the treatment of thoraco-lumbar and lumbar spinal conditions will be covered. Particular emphasis will be on the conditions seen most often in general practice-thoracolumbar disc herniations and lumbo-sacral conditions.
More information can be found in Small Animal Spinal Disorders, 2nd edition, by NJH Sharp & SJ Wheeler, Elsevier, London. Available from www.veterinary-neurology.com.
Thoracolumbar Disc Disease
Thoracolumbar disc disease is a common disorder in dogs that affects mainly chondrodystrophoid breeds. Peak incidence in these breeds is between three and six years of age. Over 50% of lesions occur at the T1/13 and T13/L1 discs and more than 85% occur between T11/12 and L2/3 inclusive. Non-chondrodystrophoid breeds are affected less frequently, usually after middle age.
Back pain and neurological deficits in the pelvic limbs are features of thoracolumbar disc disease; urinary dysfunction may occur with more severe lesions. Neurological deficits range from mild ataxia and paraparesis to paraplegia, which may be accompanied by depressed or absent deep pain sensation caudal to the lesion. There is often an associated panniculus reflex cut-off. Approximately 10-15 per cent of dogs show LMN deficits because of lesions between L3/4 and L6/7 discs.
Survey radiographs may indicate if disc disease is present but are only 60-70% accurate in identifying the exact location. CSF should be collected from all dogs prior to myelography. Either myelography or advanced imaging should be performed for definitive diagnosis. A lumbar injection is preferred for myelography because there is often considerable spinal cord swelling, which tends to cause cervical myelograms to stop cranial to the lesion. Lateral and ventrodorsal images should be taken. If it is unclear on which side the disc material is located, oblique views or a CT myelogram should be used.
CT adds accuracy and speed to the evaluation of chondrodystrophoid breeds with disc herniations. CT is non-invasive as the mineralised disc material shows clearly without the need for contrast even when it is not visible on survey radiographs. It is also usually much easier to decide what side(s) the disc material is on from CT or MRI. The increased sensitivity of CT and MRI reveal some disc herniations that are only incidental findings and that are not responsible for causing clinical signs (Figure 1).
Click on the image to see a larger view.
| Figure 1. | 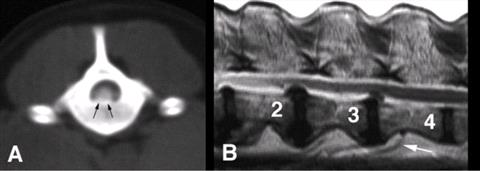
A: CT scan performed prior to myelography, shows a centrally located, mineralised mass that occupies much of the vertebral canal (arrows). B: Sagittal T2-weighted MRI through the lumbar region of an 11-year-old paraparetic Labrador with disc herniations at T12/13 to L3/4; the L2/3 and L3/4 sites are shown here. |
|
| |
Many dogs will recover from moderate neurological deficits following either nonsurgical or surgical treatment. Patients with marked deficits seen within eight hours of spinal cord injury may benefit from concomitant methylprednisolone sodium succinate (MPSS) therapy.
Strict cage rest is the overriding principle in non-surgical therapy although judicious use of analgesics or anti-inflammatory drugs may also be needed. These drugs should be withheld when feasible in order to encourage the animal to rest. The animal must rest quietly in a confined space (traveling cage size) for at least two weeks, during which time it should only be removed to urinate and defecate. A satisfactory response should be followed by a further two weeks rest and a gradual increase in activity between the fifth and eighth weeks. This is the minimum time needed for an avascular structure like the anulus fibrosus to repair. Activities like jumping should be avoided for four to six months. Animals that will not rest or are confined inadequately may fail to respond or get worse. The patient must be evaluated regularly for any deterioration, which indicates treatment failure, as does a lack of improvement within two weeks.
Although a useful initial option for some dogs with grade 1 or 2 lesions, non-surgical therapy is rarely the treatment of choice for dogs with grade 3 lesions or worse, especially if there are no financial constraints. The major long-term problem is that over one-third of dogs will suffer recurrence. Another disadvantage is that the dog can deteriorate during treatment, possibly as far as grade 5, often due to poor owner compliance.
A short course of corticosteroids without cage rest does not constitute effective nonsurgical treatment. A high proportion of dogs referred for emergency decompression have been treated in the preceding days or weeks using corticosteroids without cage confinement. Such treatment can relieve discomfort with a consequent increase in activity.
Although decompression is the surgical treatment of choice for disc disease it does demand good quality imaging. Imaging usually identifies the affected interspace but determining which side to decompress can be more problematic. Good surgical technique is needed to retrieve as much disc material as possible once the spinal cord has been exposed. Any material on the contralateral side must be removed by probing over or under the spinal cord or bilateral decompression may be needed.
Decompression by hemilaminectomy is the treatment of choice for dogs with spinal cord compression causing persistent or recurrent grade 1 signs and for most with neurological deficits. The rate of recovery is faster after decompression than after either non-surgical treatment or fenestration and there is less likelihood of residual neurological deficits. Corticosteroids provide no overall benefit when used with decompressive surgery, except possibly MPSS for dogs that present within the first eight hours of injury Concomitant fenestration should be performed at the time of the decompression. Minihemilaminectomy removes less bone than a standard hemilaminectomy but only gives good access to the ventral portion of the vertebral canal. Pediculectomy also preserves the facet joint and removes less bone than a standard hemilaminectomy.
The prognosis is very good for dogs with grade one, two, and three deficits, especially following decompression. Decompression is clearly the treatment of choice for dogs with grade five lesions, with between 60-70% recovering in most studies. Most dogs that recover regain deep pain do so within two weeks.
Lumbosacral Disease
The clinical signs seen with lumbosacral lesions differ from those seen at other locations of the spine, mainly because of the unique anatomical structure of the region. The vertebral canal in this region contains only cauda equina. The spinal cord ends within L6 vertebra in most dogs; in L7 in cats and some small dogs.
Motion in the normal lumbar spine is greatest at the lumbosacral joint. In some dogs, abnormal motion probably leads to degenerative changes such as spondylosis deformans, osteophyte proliferation and soft tissue overgrowth of the joint capsules. These degenerative changes then appear to reduce the overall range of motion. Clinical problems can arise due to compression of neural structures in the vertebral canal and intervertebral foraminae.
A number of abnormalities may combine to cause compression of the cauda equina or L7 nerve roots. These include:
 Stenosis (multilevel) of the vertebral canal.
Stenosis (multilevel) of the vertebral canal.
 Hansen Type II disc herniation at the L7/S1 intervertebral space.
Hansen Type II disc herniation at the L7/S1 intervertebral space.
 Subluxation, osteophytosis or thickening of the articular processes.
Subluxation, osteophytosis or thickening of the articular processes.
 Epidural fibrosis.
Epidural fibrosis.
 Soft tissue proliferation, usually of the joint capsule or ligamentous structures.
Soft tissue proliferation, usually of the joint capsule or ligamentous structures.
 Vascular compromise of the spinal nerves.
Vascular compromise of the spinal nerves.
 Osteochondrosis of the sacrum.
Osteochondrosis of the sacrum.
 Instability and malalignment between L7 and S1.
Instability and malalignment between L7 and S1.
The role of instability is unclear and it is difficult to quantify regardless of the imaging technique. This can pose a problem for surgical decision-making.
Lumbosacral lesions can cause pelvic limb gait abnormalities, lameness, or LMN neurological deficits. Pain is common but the signs vary depending on the nature and severity of the neurological impairment. There may be pain with no deficits; mild paresis with conscious proprioceptive deficits; or paraparesis, tail paralysis, and incontinence. Lameness in performance animals may be exacerbated by work. Incontinence results from pelvic and pudendal nerve dysfunction. Urinary incontinence is usually LMN in nature with dribbling of urine and a bladder that is easily expressed by manual pressure. Dogs with chronic degenerative lumbosacral lesions may present with non-specific clinical signs, but low back pain is quite different from that seen in thoracolumbar lesions. Diagnosis of lumbosacral disease depends on recognising the historical features and clinical signs and on a careful physical examination, which should pinpoint the source of pain.
It is advisable that the patient be anaesthetised or sedated heavily when radio-graphing the lumbosacral joint. Rotation of the spine and pelvis must be avoided. The main role of survey radiographs is to rule out neoplasia, trauma and discospondylitis. Many clinically normal dogs have radiographic abnormalities of the lumbosacral junction. Conversely, occasional dogs with lumbosacral disease will have normal survey radiographs. Neurological localisation of a patient will indicate a lesion of L4-S3 spinal cord segments. It may be possible to define the location more accurately, for example by the patellar reflex. Consideration of the diagnostic imaging of these patients frequently focuses on the LS joint alone. This policy runs the serious risk of missing lesions elsewhere in the vertebral column that are involving the L4-S3 cord segments or ascribing significance to incidental lesions of the LS joint.
Myelography can therefore be useful to assess the low lumbar region and the rest of the spinal cord. Cervical injection is preferred, as it avoids the potential for epidural contrast leakage in the area of interest. Dorsal elevation or attenuation of the column may be seen.
CT is particularly useful as it shows the vertebral canal, lateral recesses, intervertebral foramen and articular processes in cross-sectional images (Figure 2).
Click on the image to see a larger view.
| Figure 2. | 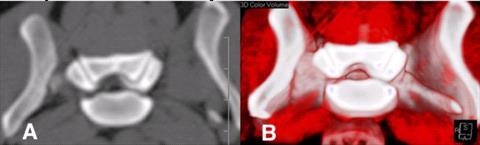
Marked foraminal compression is evident on A: Transverse CT scan and B: 3D reconstruction. Same dog as in 10.6C. |
|
| |
MRI provides better soft tissue resolution than CT as well as an ability to acquire images in multiple planes without image degradation, earlier detection of disc degeneration and evaluation of the entire lumbar spine in a single sagittal examination. Transverse images provide the best visualisation of disc or foraminal anatomy. One potential disadvantage of MRI is over-diagnosis, even by expert neuroradiologists (Figure 3).
Click on the image to see a larger view.
| IMC20882.jpg | 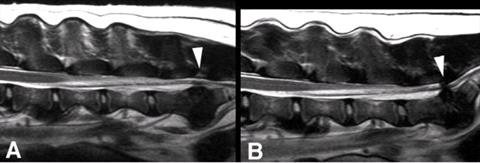
T2-weighted MRI of the lumbosacral spine of a seven-year-old Labrador with lumbosacral pain. A: Image made with the spine in flexion. There is loss of signal in the lumbosacral disc but minimal compression of the cauda equina (arrowhead). B: Image from the same dog made with the spine in extension. There is severe compression at L7/S1 caused by both disc and ligamentum flavum (arrowhead). |
|
| |
Most dogs are treated initially with rest and anti-inflammatory medication. This may be successful if pain is the main clinical sign.
Surgical treatment is indicated when nonsurgical treatment has failed, in working dogs and those with marked pain or neurological deficits. Further indications for surgery include CT or MR findings of increased soft tissue suggestive of epidural fibrosis, especially if it enhances with contrast. The choice of surgical procedure is then between dorsal laminectomy, distraction and fusion, or a combination of the two. Definitive criteria for these procedures are lacking.
Decompression of the cauda equina and spinal nerves can be achieved by dorsal laminectomy, which can be combined with foraminal decompression or even facetectomy. The anulus fibrosus should be excised once the cauda equina is retracted laterally when there is marked bulging of the disc. Routine fenestration may also be warranted. Redundant joint capsule can also be removed. Laminectomy often provides rapid relief of pain with improvement of mild gait abnormalities and minor neurological deficits; it does not address instability if this is a contributing factor. Decompression by laminectomy can be combined with fixation and fusion.
There are a number of similarities between lumbosacral disease and caudal cervical spondylomyelopathy. A rationale can therefore be made for lumbosacral distraction and stabilisation. The principle is the same, namely to open the vertebral canal and intervertebral foramen, relieve pressure on neural tissues, and prevent abnormal motion. Distraction of the dorsal aspect of L7 and S1 is achieved using screws placed through the articular processes of L7/S1 and into the body of the sacrum. Fusion is promoted by removing the articular cartilage from the facet joints and by a cancellous bone graft. This can be combined with dorsal laminectomy, especially for dogs with marked neurological deficits, severe pain, or a large disc herniation.