Introduction
In general, a biopsy should be performed before definitive treatment if the results will change the therapy or influence the owner's thoughts to treat their animals. The purpose of this lecture is to introduce image- guided biopsy techniques that are used at the Japan Small Animal Cancer Center. During the presentation, all techniques will be demonstrated by pictures and video clips.
Ultrasound-Guided Fine Needle Aspiration
1. Indications: Large-necrotizing mass that one cannot obtain diagnostic sample by blind stick, non-enlarged peripheral lymph nodes, thyroid mass, retrobulbar mass and intra-thoracic (lung mass, mediastinal mass etc.) or intra-abdominal (liver, spleen, intestine, lymph nodes etc.) mass or lesions.
2. Pros: Real-time visualization by ultrasound. Very accurate and safe.
3. Cons: Limitation of cytology
4. Precautions: Coagulopathy
5. Instruments and supplies required: ultrasound machine, various length of needles (22 or 23-gauge), extension tube, 6–12-ml syringes, pre-cleaned microscope slides, cytology stains (e.g., Diff-Quik, Wright-Giemsa, other). Sono Guide needles provide better visualization and may be helpful when the target lesion is located in deep abdomen or thorax (see Figure 1).
| Figure 1. The catheter is inserted in the mass in the urinary bladder | 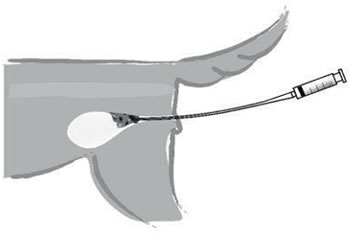
|
|
| |
6. Pearls and pitfalls
 Before the procedure, estimate or measure the depth of the target lesion so that the operator can choose a needle with the appropriate length. When the needle is inserted in close to 45 degrees, the length of the needle is approximately 1.4 times as long as the measured depth of the target lesion.
Before the procedure, estimate or measure the depth of the target lesion so that the operator can choose a needle with the appropriate length. When the needle is inserted in close to 45 degrees, the length of the needle is approximately 1.4 times as long as the measured depth of the target lesion.
 The sonographic appearance of the needle tip on the screen is a hyperechoic structure. Avoid advancing the needle if the needle tip is not visualized.
The sonographic appearance of the needle tip on the screen is a hyperechoic structure. Avoid advancing the needle if the needle tip is not visualized.
 Avoid blood dilution as much as possible. To avoid excessive blood dilutions, non-aspiration FNA technique is initially recommended. If one cannot obtain enough cells by non-aspiration FNA technique, try aspiration FNA technique. You may ask your assistant to aspirate using an extension tube so that the operator can concentrate on keeping the needle tip within the lesion. This technique is especially useful when the target lesion is less than 10 mm.
Avoid blood dilution as much as possible. To avoid excessive blood dilutions, non-aspiration FNA technique is initially recommended. If one cannot obtain enough cells by non-aspiration FNA technique, try aspiration FNA technique. You may ask your assistant to aspirate using an extension tube so that the operator can concentrate on keeping the needle tip within the lesion. This technique is especially useful when the target lesion is less than 10 mm.
 Move the tip of the needle back and forth gently within the target lesion.
Move the tip of the needle back and forth gently within the target lesion.
 Use sedation or systemic anesthesia as needed.
Use sedation or systemic anesthesia as needed.
Ultrasound-Guided Fine Needle Aspiration for Lytic Bone Lesions
1. Indication: Lytic bone lesion
2. Pros: Quick, easy, cost-effective, safe and minimal patient discomfort. The risk of pathologic fracture and wound infection are also minimal. FNA is less likely to seed neoplastic cells into the surrounding tissues.
3. Cons: Limitation of cytology; usually diagnosed as "sarcoma" and often does not allow for further classification of primary bone tumors.
4. Precaution: Coagulopathy
5. Instruments and supplies required: 22- or 23-gauge, 1–1.5-inch needles, 6–12-ml syringes, pre-cleaned microscope slides, ultrasound machine (US).
6. Technique and tips to obtain a good sample:
 After induction of anesthesia or administration of sedation, the aspiration site is clipped and surgically scrubbed.
After induction of anesthesia or administration of sedation, the aspiration site is clipped and surgically scrubbed.
 Identify the region with cortical defects by US. These areas typically appear hypoechoic.
Identify the region with cortical defects by US. These areas typically appear hypoechoic.
 A 22- or 23-gauge needle is inserted through the cortex into the medullary cavity. The author usually does not apply negative pressure to avoid blood dilution.
A 22- or 23-gauge needle is inserted through the cortex into the medullary cavity. The author usually does not apply negative pressure to avoid blood dilution.
 Remove the needle once serosanguineous fluid or blood is obtained in the hub of the needle.
Remove the needle once serosanguineous fluid or blood is obtained in the hub of the needle.
 Make multiple smears in order to increase the accuracy of diagnosis.
Make multiple smears in order to increase the accuracy of diagnosis.
Ultrasound-Guided Traumatic Catheter Biopsy for Bladder Mass
1. Indication: Urinary bladder mass
2. Pros: Tissue samples can be obtained without surgery. No risk of tumor seeding through the abdomen.
3. Cons: Difficult to obtain samples from a mass located on non-trigone area. Requires general anesthesia or at least sedation and good analgesia.
4. Precaution: Coagulopathy; biopsy specimens should be taken with caution since the bladder wall is very fragile due to the presence of the underlying disease.
5. Instruments and supplies required: 5F or 8F polypropylene urinary catheter (open-ended or closed-ended with side holes), 12-ml syringes, 18-gauge needles, pre-cleaned microscope slides, 5–10 centrifuge tubes and centrifuge, sterile saline, pipet, 10 ml of 10% buffered formalin, cytology stains (e.g., Diff-Quik, Wright-Giemsa, other), ultrasound machine (US).
6. Technique and tips to obtain a good sample:
 Identify the bladder mass with US.
Identify the bladder mass with US.
 Insert the catheter and replace urine with 10–15 ml of sterile saline. Advance the catheter forcefully into the tumor (see Figure 1). This is best accomplished with ultrasonography.
Insert the catheter and replace urine with 10–15 ml of sterile saline. Advance the catheter forcefully into the tumor (see Figure 1). This is best accomplished with ultrasonography.
 Apply suction while withdrawing the catheter (see Figure 2).
Apply suction while withdrawing the catheter (see Figure 2).
| Figure 2. The tumor is suctioned from a catheter with a side hole | 
|
|
| |
 Tissue that has been suctioned into the catheter will come out with some saline. The tissue-contained saline is centrifuged (1,500 rpm for 2–3 minutes) and the supernate is discarded.
Tissue that has been suctioned into the catheter will come out with some saline. The tissue-contained saline is centrifuged (1,500 rpm for 2–3 minutes) and the supernate is discarded.
 Repeat the procedures until enough sediment is obtained.
Repeat the procedures until enough sediment is obtained.
 All sediment are collected in one tube and filled up with 10% buffered formalin for histopathological evaluation (cell-pack).
All sediment are collected in one tube and filled up with 10% buffered formalin for histopathological evaluation (cell-pack).
 Smears are also made from the sediment for cytological evaluation before the tissue is formalinized.
Smears are also made from the sediment for cytological evaluation before the tissue is formalinized.
Other image-guided biopsy techniques including CT-guided nasal biopsy and fluoroscopic guided bone biopsy will be presented.
References
1. Ogilvie GK, Moore AS. Lower urogenital tract biopsy. In: Managing the Canine Cancer Patient: A Practical Guide to Compassionate Care. Yardley, PA: Veterinary Learning Systems; 2006:82–86.
2. Britt T, Clifford C, Barger A, et al. Diagnosing appendicular osteosarcoma with ultrasound-guided fine-needle aspiration: 36 cases. J Small Anim Pract. 2007;48):145–150.