Division of Clinical Radiology, Department of Clinical Veterinary Medicine, Vetsuisse Faculty Bern
Bern
Introduction
Diagnostic work up of musculoskeletal disorders in the dog and cat usually includes a radiographic examination, and/or other diagnostic imaging procedures. The imaging modalities are used to further characterise clinically localised problems and to differentiate disease processes: congenital and developmental disorders, degenerative, traumatic, inflammatory, neoplastic, and metabolic processes. In orthopaedic disorders of unknown origin, diagnostic imaging may be used to localise the problem, and in hereditary disorders of the musculoskeletal system they are used as screening methods.
Radiography, Ultrasonography, Scintigraphy CT or MTRI may used, alone or in any combination with the method finally selected depending on the history, clinical findings and the questions that should be addressed by the examination (Table 1). Other important criteria include the physical properties considering strengths and limitations of a method in question, of course whether or not a method is available on site, radiation hazards, and the costs (cost-effectiveness) involved. Economic aspects often decide whether an animal undergoes complete diagnostic work up and treatment or not.
| Figure 1. | 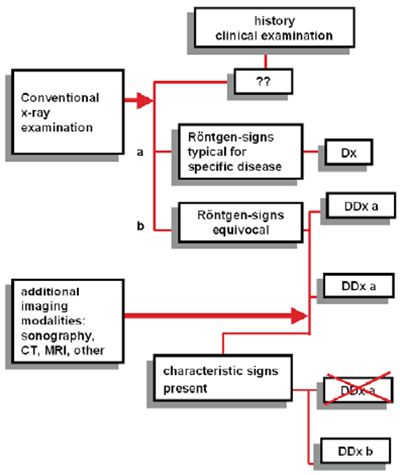
|
|
| |
Typical imaging protocol in orthopaedic disorders.
a) Conventional x-ray with radiographic signs that are typical for a specific diagnosis (e.g., flattening of humeral head for OCD). Other imaging procedures are not required or indicated.
b) An examination with equivocal findings (e.g., irregular borders and radiolucency of supraglenoid tubercle) for DDx "trauma" and "neoplasia". Additional imaging procedures (e.g., Ultrasound) are indicated. Often, a sequence of 2 or more diagnostic methods is necessary to eliminate differential diagnosis fro the initial list and to establish the correct diagnosis. Modified from: Skelettradiologie von Adam Greenspan
Table 1. Imaging modalities used in musculoskeletal disorders.
 Conventional radiography
Conventional radiography
 Includes standard projections, positional and stress views. Excellent spatial resolution: Bone architecture and morphology
Includes standard projections, positional and stress views. Excellent spatial resolution: Bone architecture and morphology
 Special procedures
Special procedures
 Arthrography--except shoulder joint rarely used
Arthrography--except shoulder joint rarely used
 Sonography
Sonography
 Musculature, tendons and ligaments; bone surface, arthrosonography US-guided fine needle and core biopsies
Musculature, tendons and ligaments; bone surface, arthrosonography US-guided fine needle and core biopsies
 Bone scintigraphy
Bone scintigraphy
 Screening method, very sensitive method for most inflammatory and neoplastic, traumatic and degenerative bone and joint pathologies, low spatial resolution, not specific for bone and soft tissue pathologies
Screening method, very sensitive method for most inflammatory and neoplastic, traumatic and degenerative bone and joint pathologies, low spatial resolution, not specific for bone and soft tissue pathologies
 Computed tomography (CT)
Computed tomography (CT)
 Structural abnormalities of bone, morphology of joints, complex fractures, extent and characterisation of bone tumours
Structural abnormalities of bone, morphology of joints, complex fractures, extent and characterisation of bone tumours
 Magnetic resonance Imaging (MRI)
Magnetic resonance Imaging (MRI)
 Any soft tissue (musculature, tendons, joints including joint capsule and ligaments, and menisci in stifle joints
Any soft tissue (musculature, tendons, joints including joint capsule and ligaments, and menisci in stifle joints
Radiography
In the imaging of musculoskeletal diseases conventional radiography still is of basic and relevant importance. The method is readily available, cost efficient and has an excellent spatial resolution. However, a lesion has to be localised by a thorough physical examination before imaging is considered, Radiography is not an adequate tool to localize a disease process and the sensitivity of radiography depends on the disease process and the structure involve. Abnormal findings may not be associated with clinical signs and may be misleading. For example, mildly dysplastic and osteoarthritic hip joints are clinically silent in most dogs. Radiographic standard projections usually include at least two projections. However these are often not sufficient for a radiographic diagnosis: in particular, a thorough radiographic examination of joints often includes flexed and extended views from different angles. An example is the radiographic protocol in elbow dysplasia, which may include up to 6 or 7 projections, depending on the disease process in question. Positional and stress radiographs may be used to confirm or eliminate joint instability. Invasive radiographic methods, such as arthrography, are mostly used in the shoulder joint; however, with increasing availability and expertise of other imaging techniques arthrography becomes less important.
Thorough knowledge of the radiographic anatomy including species and breed specific variations, age dependent changes and the skills in interpreting of a radiograph are of equal importance as the radiographic technique. Characterization of bone lesions not only includes the description of the abnormality, but also the distribution and localisation in the skeleton, localisation in a specific bone, and so on (Table 2). Diagnosis is based on description, the ID of patient and clinical signs
Table 2. Interpretation criteria for skeletal radiographs.
 Radiographic abnormality
Radiographic abnormality
 Alteration of architecture (size, shape, border) and proportion, of opacity and structure (osteoporosis/atrophy, osteolysis, osteosclerosis, osteopetrosis)
Alteration of architecture (size, shape, border) and proportion, of opacity and structure (osteoporosis/atrophy, osteolysis, osteosclerosis, osteopetrosis)
 Intraskeletal distribution
Intraskeletal distribution
 Generalized, (oligo-) polyostotic, monostotic
Generalized, (oligo-) polyostotic, monostotic
 Localisation
Localisation
 Within the skeleton: bone or bones affected
Within the skeleton: bone or bones affected
 Within the bone longitudinal: proximal or distal epiphysis, physis (growth plate), metaphysis, and/or diaphysis
Within the bone longitudinal: proximal or distal epiphysis, physis (growth plate), metaphysis, and/or diaphysis
 Cross sectional: bone marrow, endosteum, compact bone, periosteum, soft tissues
Cross sectional: bone marrow, endosteum, compact bone, periosteum, soft tissues
 Complications
Complications
 e.g., metastases, effects on other structures/joints
e.g., metastases, effects on other structures/joints
 Aggressivity of a lesion
Aggressivity of a lesion
Bone scintigraphy
Bone scintigraphy is often used as screening method in lameness in horses and less commonly in small animals in order to localize an occult skeletal lesion, and to screen for metastases in tumour cases. Scintigraphy reflects metabolic activity. An injection of 99m Tc-Sc-methylendiphosphate at a dosage of 16.3 MBq/kg bodyweight is required for osseous radiolabeling. 99mTc produces gamma radiation with an energy of 140 keV, which collected and visualized using a gamma-camera. The distribution can be registered as an angiographic study immediately after injection, a pool phase some minutes, and the metabolic phase 2-3 or more hours after injection (Figure 2). In small animals a maximum of 300 k-counts per region are recorded. Comparing the metabolic activity of a specific structure to the controlateral body part is essential. Increased or decreased activity reflects abnormal perfusion and/or metabolism.
| Figure 2. | 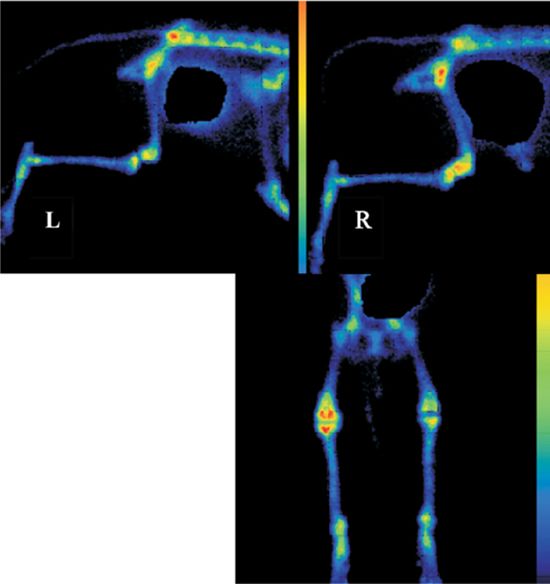
|
|
| |
Bone scan of a dog with clinically not clearly localized lameness of the right hindlimb. Equal orientation of the two hindlimb--scans facilitates the comparison to the controlateral part. Note the difference in activity of the two stifle-joints.
Kidneys and urinary tract eliminate unattached tracer-particles. Therefore image editing is needed to correct the highly active urine in the urinary bladder overlaying less active bony structures. In the present bladder-activity is suppressed by imaging software (black spot).
Bone scan (dorsal view) of the same dog: metabolic activity of separate regions of the hindlimbs can be compared directly positioning of the legs is symmetric. The right stifle shows intensive enhancement clearly distinct from the left stifle.
red: peak of activity; dark blue: lowest activity
Sonography
Standard method for soft tissue diagnostics, particularly for abdominal examinations where it is often performed as single examination. To some extent this is also true in musculoskeletal disorders, e.g., for tendinal lesions in the horse. In small animals, sonography most often is used as an adjunct diagnostic tool. Lesions of the bones have to be ruled out by radiography. Clinically relevant examinations include tendons (biceps tendon, Achilles tendon) and tendon sheath's after trauma or control after surgery, joints (shoulder joint, stifle, hip joint) in order to differentiate between fluid accumulation and soft tissue proliferations (e.g., suspicion of neoplasia), US controlled assessment of joint-stability (alternatively to stress radiographs), sonographic examination of post traumatic musculature (ruptures, hematoma), suspicion of tumour or abscess, US guided FNA or biopsy.
| Figure 3. | 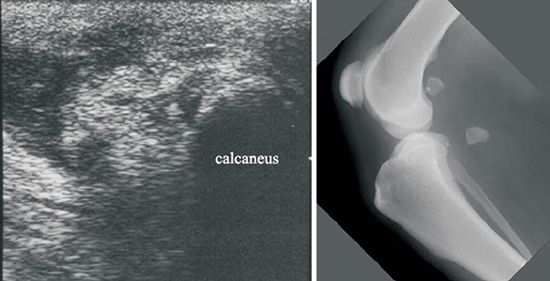
|
|
| |
Left: Sonography of a dog showing clear signs of a ruptured Achilles tendon which was verified and repaired surgically. Only after the dog did not improve clinically, a radiographic examination was performed. The lateral projection of the stifle joint revealed a distally dislocated sesamoid bone of the lateral gastrocnemius muscle, a radiographic sign of an avulsion of the respective muscle.
Computed Tomography (CT) and Magnetic Resonance Imaging (MRI)
Both techniques are becoming very popular also in veterinary medicine. Whenever available, they are used as additional diagnostic tools whenever radiographic or sonographic findings are equivocal, as an alternative for arthroscopy, or for further characterisation (extent and nature of a lesion) of a known lesion. In general CT is used primarily for bone disorders; MRI, on the other hand, is the method of choice for soft tissue imaging. CT is useful to visualise complicated fractures (joints, pelvis) preoperatively--a three dimensional CT-reconstruction can be very helpful for the surgeon planning the surgery. Furthermore CT is used as gold standard to explore malformations and developmental disorders of complex joints: The sensitivity of radiographs of a fragmented medial coronoid process is below 50%, the sensitivity and specificity of a CT is close to 100%. Characterisation and assessment of the extent of primary bone tumours or bone affecting tumours preoperatively or pre-radiation-therapy are other indications for CT.
MRI has the highest contrast resolution for soft tissues and has become method of choice in neurological disorders. In orthopaedic disease MRI is useful for soft tissue pathology, e.g., imaging of internal derangement of joints such as the stifle-joint. Ruptured cruciate ligaments, tears and other pathologies of the menisci, disease of articular cartilage, and joint capsule are readily imaged (Figure 4). By choosing the appropriate planes and sequences, MRI is sensitive and specific for many musculoskeletal pathologies. Since increase in cell- or fluid content within bones can also be seen in MRI, bone-tumors, osteomyelitis and post-traumatic bone marrow edema are also detectable.
| Figure 4. | 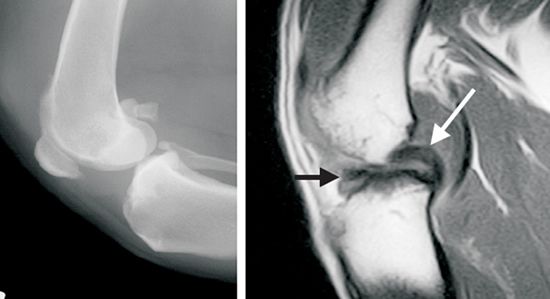
|
|
| |
Llateral radiograph (left) and saggital plane section of a stifle-joint with ruptured cranial cruciate ligament. Radiological findings are unspecific. With MRI the intact caudal cruciate ligament (white arrow) and the thickened remainder of the ruptured cranial cruciate ligament are visible (black arrow).
References
1. Carrig, C. B. 1997. Diagnostic imaging of osteoarthritis. Vet. Clin. North Am. Small Anim Pract. 27: 777-814.
2. Davis GJ., Kapatkin AS., Craig LE., Heins GS., Wortman JA: Comparison of radiography, computed tomography, and magnetic resonance imaging for evaluation of appendicular osteosarcoma in dogs; J Am Vet Med Assoc. 2002 220(8): 1171-6.
3. Fitch RB., Wilson ER., Hathcock JT., Montgomery RD: Radiographic, computed tomographic and magnetic resonance imaging evaluation of a chronic long digital extensor tendon avulsion in a dog; Vet Radiol Ultrasound. 1997 38(3): 177-81.
4. Gemmill TJ.; Mellor DJ., Clements DN., Clarke SP., Farrell M., Bennett D., Carmichael S: Evaluation of elbow incongruency using reconstructed CT in dogs suffering fragmented coronoid process; J.Small Anim Pract. 2005; 46(7): 327-33.
5. Hoskinson, J. J. and R. L. Tucker. 2001. Diagnostic imaging of lameness in small animals. Vet. Clin. North Am. Small Anim Pract. 31: 165-80, vii.
6. Liptak JM, Pluhar GE, Dernell WS, Withrow SJ:Limb-Sparing Surgery in a Dog with Osteosarcoma of the Proximal Femur, Veterinary Surgery 2005; 34: 71-77.
7. Thrall DE: Textbook of Veterinary Diagnostic Radiology 4th edition. W.B. Saunders Company, 2002.
8. Wallack ST., Wisner ER., Werner JA., Walsh PJ., Kent MS., Fairley RA., Hornof WJ: Accuracy of magnetic resonance imaging for estimating intramedullary osteosarcoma extent in pre-operative planning of canine limb-salvage procedures; Vet Radiol Ultrasound 2002 43(5): 432-41.
9. see also manuscript on MRI of the musculoskeletal system