The Practice Success Prescription: Team-Based Veterinary Healthcare Delivery by Drs. Leak. Morris Humphries
Thomas E. Catanzaro, DVM, MHA, FACHE, DACHE
"You never get a second chance to make the first impression"
You have graduated, you have passed the boards for veterinarians and technicians, while managers achieve CVPM via the VHMA, and you have finally found a practice that you think is what you want, and the owner wants you. You must walk through the door of that practice now, and you will make the first impression as a "new" team member.
You know in your heart that you are expected to be a leader in case management, yet you also need to be a follower of the practice's standards of care, and contribute to the continuity of care of patients you have never seen, owned by clients you have never met, and with a staff who probably has many more years of practical experience than you. Which leads us into the next topic.
Whatcha Goin'T'Do?
Hopefully, you have been directed into a Toastmasters or a Dale Carnegie course during your last year of school. If you have developed/learned communication skills, life will be far easier in your new work environment. Maybe you have read Crucial Conversations by Patterson, et. al., and have a skill set for leading participative facilitated discussions. Then again you may have been one of those "gunners", who only studied for tests, and let the life skills ride during your school years. Regardless, the first ninety days in a practice have many similarities, and the savvy "new Doc" will address the new environment, using a sane and progressive integration system.
The following list applies to the newly hired graduate. However, you long-time practitioners will want to review the following information yourselves. You never know when you might need it!
 Pre-day one: Make an agreement with your employer that you get thirty days of non-productive time to learn the system and strengths. You may get involved in some wellness cases, but please resist trying to jump in with both feet. se the "short list" offered below for the first month to "negotiate" your initial orientation and primary care development time. Some may believe they "know it all", but experience has shown the listed items are usually very practice-specific, so make yourself valuable by becoming a student of the practice's systems and expectations.
Pre-day one: Make an agreement with your employer that you get thirty days of non-productive time to learn the system and strengths. You may get involved in some wellness cases, but please resist trying to jump in with both feet. se the "short list" offered below for the first month to "negotiate" your initial orientation and primary care development time. Some may believe they "know it all", but experience has shown the listed items are usually very practice-specific, so make yourself valuable by becoming a student of the practice's systems and expectations.
 Day one: Dress like a practice doctor. Follow practice standards. Be careful of being a sparkling clothes horse, or a street person dress-down, ensure your hygiene is smell-worthy, and put a smile on your face. When being introduced, don't be cute, be sincere. Learn staff names, and associate names with practice skill areas or areas of personal pride. As applicable, get personal copies of the mission statement, vision, core values, practice philosophy, employee manual, and other baseline documents. Read and learn them.
Day one: Dress like a practice doctor. Follow practice standards. Be careful of being a sparkling clothes horse, or a street person dress-down, ensure your hygiene is smell-worthy, and put a smile on your face. When being introduced, don't be cute, be sincere. Learn staff names, and associate names with practice skill areas or areas of personal pride. As applicable, get personal copies of the mission statement, vision, core values, practice philosophy, employee manual, and other baseline documents. Read and learn them.
 Week one: Ensure you get a practice rotation established, so you can spend at least one full shift in each practice zone, learning what is done and how it is done. Ask questions about what staff wants you to do in the course of a patient episode. Solicit from "womb-to-tomb" alternatives and expectations.
Week one: Ensure you get a practice rotation established, so you can spend at least one full shift in each practice zone, learning what is done and how it is done. Ask questions about what staff wants you to do in the course of a patient episode. Solicit from "womb-to-tomb" alternatives and expectations.
 Month one: Become a fixture in the treatment room. Do not try to change or challenge anything, until you learn the "how" and "why" of the current operations. In short, continue being a great student this month. Just ask questions and learn how they want things done. Ask the staff to "help you learn the practice methods" for:
Month one: Become a fixture in the treatment room. Do not try to change or challenge anything, until you learn the "how" and "why" of the current operations. In short, continue being a great student this month. Just ask questions and learn how they want things done. Ask the staff to "help you learn the practice methods" for:
 Maintaining staff harmony (usually a core value).
Maintaining staff harmony (usually a core value).
 Review staff training protocols and programs.
Review staff training protocols and programs.
 Pre-emptive pain scoring program(s) and protocols.
Pre-emptive pain scoring program(s) and protocols.
 Inpatient pain scoring program(s) and protocols.
Inpatient pain scoring program(s) and protocols.
 White board use, or the use of the treatment room flow sheet.
White board use, or the use of the treatment room flow sheet.
 Bathing patients. You learn best by doing it. Use Hydro-surge or equivalent.
Bathing patients. You learn best by doing it. Use Hydro-surge or equivalent.
 Hospital ward monitoring systems, and cage card use.
Hospital ward monitoring systems, and cage card use.
 Determining hospitalization levels.
Determining hospitalization levels.
 Respecting nursing rounds.
Respecting nursing rounds.
 How IPNT schedules inpatient doctor(s), and staying on time.
How IPNT schedules inpatient doctor(s), and staying on time.
 Operating the laboratory equipment and in-house lab kit tests.
Operating the laboratory equipment and in-house lab kit tests.
 Setting up fecals.
Setting up fecals.
 Outside lab form completion terminology/protocols.
Outside lab form completion terminology/protocols.
 CBC procedures.
CBC procedures.
 UA and ERD procedures.
UA and ERD procedures.
 Staining slides.
Staining slides.
 Cytology procedures.
Cytology procedures.
 Catheterization. Be a holder and watch first.
Catheterization. Be a holder and watch first.
 Learn risk assessment scoring required for all admissions.
Learn risk assessment scoring required for all admissions.
 IV therapy and IOF protocols.
IV therapy and IOF protocols.
 Radiology positioning.
Radiology positioning.
 Radiograph processing.
Radiograph processing.
 Telemedicine capabilities/agreements.
Telemedicine capabilities/agreements.
 Ultrasound/endoscope protocol(s), as applicable.
Ultrasound/endoscope protocol(s), as applicable.
 In-house ECG procedures.
In-house ECG procedures.
 Hospitalization protocols.
Hospitalization protocols.
 Nutritional grading of inpatients.
Nutritional grading of inpatients.
 Body condition scoring for outpatients.
Body condition scoring for outpatients.
 Learn dental grading, all four levels.
Learn dental grading, all four levels.
 Dental prophy: grade 1+ and Grade 2+ dentals.
Dental prophy: grade 1+ and Grade 2+ dentals.
 Oral surgery and periodontal care: grade 3+ and grade 4+ dentals.
Oral surgery and periodontal care: grade 3+ and grade 4+ dentals.
 Surgical pack preparation.
Surgical pack preparation.
 Pre-surgical patient surveillance standards.
Pre-surgical patient surveillance standards.
 Pre-anesthesia techniques and protocols.
Pre-anesthesia techniques and protocols.
 Patient induction protocols.
Patient induction protocols.
 Patient anesthetic monitoring expectations.
Patient anesthetic monitoring expectations.
 Start doing spays and neuters.
Start doing spays and neuters.
 Gain surgery speed and techniques, using practice resources.
Gain surgery speed and techniques, using practice resources.
 Scrub in and assist in other surgeries.
Scrub in and assist in other surgeries.
 Recovery procedures.
Recovery procedures.
 Patient discharge instructions.
Patient discharge instructions.
 Understanding of computer, travel (circle) sheet, and category use.
Understanding of computer, travel (circle) sheet, and category use.
 Planning the next contact, using the three Rs one hundred percent: Recheck, Recall, and Remind.
Planning the next contact, using the three Rs one hundred percent: Recheck, Recall, and Remind.
 When treatment room is slow, shadow outpatient doctor(s):
When treatment room is slow, shadow outpatient doctor(s):
 Understand the OPNT asymmetry exam.
Understand the OPNT asymmetry exam.
 Accept the documentation shorthand expectations.
Accept the documentation shorthand expectations.
 Become confident. Use "need" ([ ]), instead of "recommend".
Become confident. Use "need" ([ ]), instead of "recommend".
 Learn to deliver "two yes" option narratives.
Learn to deliver "two yes" option narratives.
Respect the S-O-A-P (H-E-A-P) formats of the practice.
 Review the "assessment" to "problem list" techniques.
Review the "assessment" to "problem list" techniques.
 Understand the importance of admit or discharge decision, after ten minutes of doctor's consultation.
Understand the importance of admit or discharge decision, after ten minutes of doctor's consultation.
 Work outpatient for wellness cases on a Saturday morning.
Work outpatient for wellness cases on a Saturday morning.
 Understand practice's competency and productivity standards.
Understand practice's competency and productivity standards.
 Develop an agreement for seeing new clients with wellness patients.
Develop an agreement for seeing new clients with wellness patients.
 Learn to cherish the staff as valuable practice assets.
Learn to cherish the staff as valuable practice assets.
 Seek constructive feedback from the employer on a weekly basis.
Seek constructive feedback from the employer on a weekly basis.
 Month two: Become an outpatient resource. Continue a dependable surgery schedule for spays and neuters, and possibly a few other procedures in which you have confidence. Continue to not change or challenge anything, until you learn the "how" and "why" of the current operations. Continue being a great student for outpatient procedures.
Month two: Become an outpatient resource. Continue a dependable surgery schedule for spays and neuters, and possibly a few other procedures in which you have confidence. Continue to not change or challenge anything, until you learn the "how" and "why" of the current operations. Continue being a great student for outpatient procedures.
 This month: Learn the narratives and preferences of the practice, often called the standards of care, and ensure you are meeting the continuity of care expectations of the doctors and staff in your documentation. Ask often for feedback from the medical director/owner on impressions of your team support and contributions to staff harmony. Learn how "day care" admissions can improve patient care, while providing you an often-needed, second opinion. In many companion animal practices, experienced providers have about a forty percent day admit rate from outpatient cases for such things as radiographs, ear flushes, full chemistry cases, VetScope cases, etc.
This month: Learn the narratives and preferences of the practice, often called the standards of care, and ensure you are meeting the continuity of care expectations of the doctors and staff in your documentation. Ask often for feedback from the medical director/owner on impressions of your team support and contributions to staff harmony. Learn how "day care" admissions can improve patient care, while providing you an often-needed, second opinion. In many companion animal practices, experienced providers have about a forty percent day admit rate from outpatient cases for such things as radiographs, ear flushes, full chemistry cases, VetScope cases, etc.
Attitude Counts
The good doctor knows that "day admits" depend on the staff competencies. A great doctor encourages and supports the staff in developing day admit competencies. Day admit competencies means the staff have been trained and are trusted to do most all of the routine imaging procedures, IV procedures, ear flushes, laboratory samples, etc., so results are ready for the doctor's assessment. The terms of employment for new doctors are the same for all other staff members:
 Team fit: Maintains and supports practice harmony efforts.
Team fit: Maintains and supports practice harmony efforts.
 Competency: Dependability for producing expected outcomes.
Competency: Dependability for producing expected outcomes.
 Productivity: Staying on schedule. Speed comes with time.
Productivity: Staying on schedule. Speed comes with time.
 Patient advocacy: Speaking for what the pet "needs".
Patient advocacy: Speaking for what the pet "needs".
 Client-centered service: Listening and responding to their wants.
Client-centered service: Listening and responding to their wants.
For a staff doctor, there are additional "terms of employment", since they lead a healthcare delivery team:
 Respect: Maintaining consistency with staff, clients, doctors, and self.
Respect: Maintaining consistency with staff, clients, doctors, and self.
 Responsibility: Based on strengths. Give others meaningful tasks.
Responsibility: Based on strengths. Give others meaningful tasks.
 Recognition: Individual and specific, in public, and often.
Recognition: Individual and specific, in public, and often.
 Reliability: Accept credit for success and failure. No blaming.
Reliability: Accept credit for success and failure. No blaming.
 Patient advocacy: Speaking for what the pet "needs"
Patient advocacy: Speaking for what the pet "needs"
 Client-centered service: Listening and responding to the client's wants.
Client-centered service: Listening and responding to the client's wants.
Yes dear graduates, the last two elements above are stated twice. That is how important they are. We know that primary care is not at the high end of training at most veterinary teaching hospitals. As such, allow me to share with you the secret triad of client bonding. Commit these to memory and strive to accomplish them with every case:
 Allow no Pain.
Allow no Pain.
 Allow no puking, peeing, or pooping in the home
Allow no puking, peeing, or pooping in the home
 Tell the client how to feed the animal. Never tell a client not to feed the animal (NPO).
Tell the client how to feed the animal. Never tell a client not to feed the animal (NPO).
The emergency and critical literature tells us that in traditional NPO cases, a five to ten ml glucose lavage, keeps the gastric flora more viable, thereby enhancing recovery. It concurrently allows the pet stewards to feel they are doing something. This is similar to the clear broth or clear liquids guidance given to mothers. No intelligent doctor ever tells a mom they cannot feed their child!
Final Point of Clarification
The first point of clarification offered in this chapter was:
If you cannot accept these quality medicine, team-based, baseline principles, this chapter is NOT designed for your practice. This information is designed for those who want to differentiate their practice with client-centered, team-based, quality healthcare delivery.
If you are still thinking, "How will this effect my average client transaction (ACT)?", you have missed the point. Simple math again. If you have an act of $134, and it drops to $99, is that "good" or "bad"? When you ex-sanguinate the wallet at each visit, so the client only comes in once or twice a year at $134, does that earn you more or less than that patient coming in four or five times a year at $99? For those of you who are bad at math, two times $134 equals $268, while four times $99 equals $396, a difference of $128, mostly pure net, since fixed overhead did not change.
In a recessionary economy, or tight household budget, which would make your clients feel better with each visit, especially if the interim nursing visits were without doctor consultations?
If you are still thinking act and gross instead of "visits per pet per year" and net, or if you still beat on your associates about act as a key measurement of production, you have missed the point of this entire discussion, and probably need an outside set of eyes for a patient care consultation.
Become a Valuable Asset
The new doctor is supposed to become productive as soon as possible. You must learn what this means for your practice in both personal caseload carried and the income you need to generate to support yourself and the staff you depend on for continuity of care.
It is important that you learn to stay on schedule, as well as schedule personal issues outside the practice day. The most productive doctors leverage their time by using the staff as critical resources on their healthcare delivery team.
They understand what the staff members can do and trust them to do it well. If a staff member does not know how to do a support function, time is taken to coach the staff member to a level of competency and trust.
Doctors who accolade staff members in public, and coach in private, become respected team members. Doctors who give credit and take blame become respected leaders. The practice owners who remember the reason they applied to get into veterinary school, and understand that the staff and doctors are in this profession for the "warm fuzzies" that come with caring for animals, can motivate the team with:
1. Inviolate core values.
2. Quality, team-based, healthcare delivery.
3. Clear standards of care.
Summary
Become a client-centered practice. Promote patient advocacy. Establish a fee schedule based on nationally known fees, not the guy down the street. Build pride in the staff by ensuring they know where you are to the national fees.
Standard Care with VPI® is at approximately fifty percent expected fees, and Superior Care with VPI® is at approximately eighty percent expected fees. They are "indemnity insurance" programs, so they "risk share" and have ceilings on reimbursements.
The days of a doctor-centered practice are coming to an end, as are the days of below-standard fees. The technology and scope of services for tomorrow cannot be procured with yesterday's discounting habits. Practices deserve to be able to pay their staff a living wage, and new graduate veterinarians deserve adequate income to pay off six-digit school loans.
Affordable pet care is an extension of the human-animal bond mission, as well as the medical charter, "First, do no harm". We have a "social contract" to help the client find alternative ways to pay for the needed animal healthcare services before the crisis occurs. We have a calling. It started as "tend to the animals of the land", though it never said for free or at a loss. To do less, with services and fee-for-services, is to ignore our sacred duty as veterinary professionals.
The techniques to apply the human/companion animal bond to daily practice, as discussed here, are not all-inclusive, nor are techniques fail-safe methods to build a client-practice bond. The sincere sharing of feelings will be accepted by the majority of our clients and, most often when exhibited appropriately and sincerely, will cause a client to keep a bond with the practice, even after a pet's untimely death. Put yourself in the client's position and give the compassion that the stressing situation requires. Understand that awareness of the human-companion animal bond belongs in practice, as well as nursing homes, or other pet-facilitated therapy programs.
| Figure 13: Reality Check Diagram | 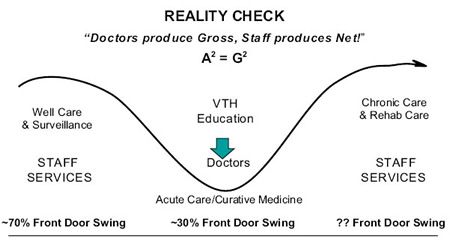
|
|
| |
It is important to note that while pet parents come in many varieties, the basic reality is that most all pet care comes from discretionary spending dollars. As a profession, we are moving away from one visit a year and super ex-sanguination of the wallet.
In the above diagram we show a front door swing rate curve, and would like to point out that after the two life cycle consultations a year by the doctor, the majority of well care is scheduled husbandry by the nursing staff, which includes nutrition, vaccinations, parasites, dental hygiene, behavior management, surveillance testing, etc. Also, in chronic care, sequential labs, weight surveillance, cardiac monitoring, lump surveillance, etc., is also predominantly a staff function. In the center of the curve is the doctor's knowledge/skill territory of expertise and excellence: diagnose, prescribe and surgicate.
In our experience, clients (pet parents) like coming into their veterinary practice more often, especially if the service is economically conducted by a caring nursing staff. In a series of visits, the total value of each patient in increased:
 Two doctor consultations a year (life cycle consultation) instead of one.
Two doctor consultations a year (life cycle consultation) instead of one.
 Eight-five percent of adult animals need some form of dental care. Seven to ten days after a dental cleaning, clients come back for a courtesy nursing appointment to discuss dental hygiene and dental diets. After four to six months, pet parents come back for a courtesy nursing appointment to have dental hygiene check.
Eight-five percent of adult animals need some form of dental care. Seven to ten days after a dental cleaning, clients come back for a courtesy nursing appointment to discuss dental hygiene and dental diets. After four to six months, pet parents come back for a courtesy nursing appointment to have dental hygiene check.
 Fifty percent of animals need a quality nutrition program, and since animals on quality diets live twenty-two months longer (Purina Research), all pets deserve to be on premium diets. Most feeding trials, such as Slimmer/Fat Burner Programs, take three to five visits with the attending nutritional counselor.
Fifty percent of animals need a quality nutrition program, and since animals on quality diets live twenty-two months longer (Purina Research), all pets deserve to be on premium diets. Most feeding trials, such as Slimmer/Fat Burner Programs, take three to five visits with the attending nutritional counselor.
 We have many parasite prevention medications, and some of these even prevent heart worms.
We have many parasite prevention medications, and some of these even prevent heart worms.
 Some states have changed their Practice Acts to allow technicians to administer vaccines. With extended DOI vaccines, we must separate immunization programs from the doctor's life cycle consultation.
Some states have changed their Practice Acts to allow technicians to administer vaccines. With extended DOI vaccines, we must separate immunization programs from the doctor's life cycle consultation.
 Fecals, sequential labs, urine screens, etc., are simple, sample drop offs, or blood draws, and do not require a doctor to accept/draw the sample.
Fecals, sequential labs, urine screens, etc., are simple, sample drop offs, or blood draws, and do not require a doctor to accept/draw the sample.
Please note: the number of visits per year per pet cannot be just one and still handle "all of the above", plus genetic predisposition monitoring, client education, and follow-up surveillance care.
Software, like Fair Fees®, has already been designed to establish fees based on staff versus doctor time. Meanwhile, integrated software, like the RxWorks® Production Pack©, has added overhead, staff numbers and compensation, doctor numbers and costs, plus a profit target, into a pre-programmed workload procedures listing, so a practice-specific fee schedule can be automatically driven, which is then adjustable by the practice leadership.
The savvy practice leadership has discovered that at about $350,000 to $450,000 production, a doctor-centered practice starts to hit a capacity ceiling, thereby capping the doctor's income potential at about twenty percent of production. A team-based practice doubles to triples the per doctor production, thereby increasing the doctor's income potential at about twenty percent of production by two to three-fold. The same increases in staff compensation is also seen, since a mature practice's total compensation budget, those W-2 wages for doctors, management and staff, needs to be less than forty-three percent of gross to balance the budget.
Team-based healthcare delivery is smart for reduced stress, advantageous for monetary returns, and extremely rewarding to the staff members who joined this profession as a calling. Good Medicine is Good Business!