The Practice Success Prescription: Team-Based Veterinary Healthcare Delivery by Drs. Leak. Morris Humphries
Thomas E. Catanzaro, DVM, MHA, FACHE, DACHE
Every practice leader needs to be aware of the evolving veterinary medicine and healthcare delivery practices. No longer is curative medicine pricing, to fix a specific problem at a specific time, an acceptable approach for wellness surveillance, which is a recurring workload. Recurring healthcare delivery seen in wellness surveillance programs is protocol-based and mostly staff-driven, whereas curative medicine invokes the doctor's skill, knowledge, and experience at every turn.
To cause the veterinary paradigm changes needed, we have developed this "capper" reference text. We have tried to bring together all the aspects of team-based healthcare delivery. In this reference, we present a single-source reference to better meet the charter Catanzaro & Associates, Inc., presented as a consulting firm over ten years ago. Simply, to be successful, the veterinary practice leadership must actively embrace the change process: reinvent, rethink and rebuild. Concurrently, we offer some basic new concepts to allow the veterinary practice evolution to move more rapidly forward, including five major perspectives:
1. Functional Zoning of the Veterinary Facility
 Staff run the reach zone and are accountable for recurring improvements.
Staff run the reach zone and are accountable for recurring improvements.
 Staff schedules clients per established protocols, and doctors respect the staff and schedule at all times.
Staff schedules clients per established protocols, and doctors respect the staff and schedule at all times.
 When assigned to a specific zone, neither staff nor doctors disappear. They are accountable to that zone to finish the workload as scheduled.
When assigned to a specific zone, neither staff nor doctors disappear. They are accountable to that zone to finish the workload as scheduled.
 Client Relations is accountable for keeping the front door swinging, and has a telephone team separate from the front desk greeters and routers.
Client Relations is accountable for keeping the front door swinging, and has a telephone team separate from the front desk greeters and routers.
 Outpatient Nurse Technicians, as nurse is a client-friendly term, provide a high level of communication and hospitality, as well as continuity of care.
Outpatient Nurse Technicians, as nurse is a client-friendly term, provide a high level of communication and hospitality, as well as continuity of care.
 Inpatient teams are built around a skilled technician with an assistant, never a second technician. No one ever pulls the assistant away from the Inpatient Nurse Technician.
Inpatient teams are built around a skilled technician with an assistant, never a second technician. No one ever pulls the assistant away from the Inpatient Nurse Technician.
 Animal caretakers are entry level positions, accountable for animal welfare, as stated in Title 9, Code of Federal Regulations (CFR), and facility maintenance.
Animal caretakers are entry level positions, accountable for animal welfare, as stated in Title 9, Code of Federal Regulations (CFR), and facility maintenance.
 Doctors are assigned to a zone by half-day increments, reporting to the accountable staff and agreeing to maintain the established schedule priorities and healthcare delivery systems (standards of care).
Doctors are assigned to a zone by half-day increments, reporting to the accountable staff and agreeing to maintain the established schedule priorities and healthcare delivery systems (standards of care).
2. Multi-Tasking Training Techniques (mt3)
 One doctor plus one nurse work a minimum of two consult rooms, with a pharmacy float assistant as a second pair of hands and pill counter.
One doctor plus one nurse work a minimum of two consult rooms, with a pharmacy float assistant as a second pair of hands and pill counter.
 Outpatient doctor never has a single column in an appointment log.
Outpatient doctor never has a single column in an appointment log.
 Inpatient has multiple, concurrently operating, work stations, including dental hygiene, laboratory, surgery, and imaging. The central inpatient team supports induction and recovery for the various stations, as needed.
Inpatient has multiple, concurrently operating, work stations, including dental hygiene, laboratory, surgery, and imaging. The central inpatient team supports induction and recovery for the various stations, as needed.
 Treatments, such as bid, tid, and qid, monitoring, fluid therapy, and Risk Level 1, DG1+ or DG2+ are nursing functions.
Treatments, such as bid, tid, and qid, monitoring, fluid therapy, and Risk Level 1, DG1+ or DG2+ are nursing functions.
 Staff own seventy percent of the three Rs: recall, recheck, remind.
Staff own seventy percent of the three Rs: recall, recheck, remind.
3. A2 = G2 Paradigms must be Changed
 Quality Assurance (QA) spot checks outcome for sameness.
Quality Assurance (QA) spot checks outcome for sameness.
 Quality Control (QC) spot checks process for sameness.
Quality Control (QC) spot checks process for sameness.
 QA and QC ensure system replication, while concurrently preventing change and evolution by their very nature.
QA and QC ensure system replication, while concurrently preventing change and evolution by their very nature.
 Continuous Quality Improvement (CQI) means each person makes tomorrow better than today, a concept that must overlay all QC and QA programs for the benefit of staff, practice, clients, and/or patients.
Continuous Quality Improvement (CQI) means each person makes tomorrow better than today, a concept that must overlay all QC and QA programs for the benefit of staff, practice, clients, and/or patients.
4. Staff Becomes Accountable for Outcomes!
 Wellness surveillance is a team function of client-centered patient advocacy.
Wellness surveillance is a team function of client-centered patient advocacy.
 Wellness healthcare delivery is a staff function, centering on husbandry and quality of life for pets within the family.
Wellness healthcare delivery is a staff function, centering on husbandry and quality of life for pets within the family.
 Doctor-heavy practices will continue to have a false ceiling on the earning potential of doctors and staff.
Doctor-heavy practices will continue to have a false ceiling on the earning potential of doctors and staff.
 Staff-operated facilities will allow the doctors to center on diagnosing, prescribing and doing surgery, while maintaining enhanced client communications concerning the value of services offered.
Staff-operated facilities will allow the doctors to center on diagnosing, prescribing and doing surgery, while maintaining enhanced client communications concerning the value of services offered.
5. Every Practice has Three Primary Income Centers Available to Them
 Preventive medicine: Vaccines, fleas, ticks, heartworms, parasites, spay/neuter, and maybe even some dental and nutritional wellness care.
Preventive medicine: Vaccines, fleas, ticks, heartworms, parasites, spay/neuter, and maybe even some dental and nutritional wellness care.
 Curative medicine and surgery: Is twenty to thirty percent of the case load in most mature practices, and it is very difficult to change this ratio.
Curative medicine and surgery: Is twenty to thirty percent of the case load in most mature practices, and it is very difficult to change this ratio.
 Wellness surveillance: Life cycle and breed-dependent needs, an untapped workload center in most practices, mainly because it is heavy in husbandry and needs staff trained to a level of being trusted.
Wellness surveillance: Life cycle and breed-dependent needs, an untapped workload center in most practices, mainly because it is heavy in husbandry and needs staff trained to a level of being trusted.
The above is easier stated and implemented. We have published twelve previous texts, and about thirty VCI® Signature Series Monographs. We have seen our nomenclature be absorbed into the profession, and many of our principles and systems adopted by other consultants and practices as their own discoveries. We have seen incremental changes as people embrace our philosophy and concepts of operational excellence. To appreciate the full impact, the concept flow must be equally embraced, with each step fully absorbed and integrated into daily operations:
 Vision: A five-to-ten-year statement of what is over the horizon. Something so powerful that it motivates the team and brings it back to the course set by the practice after times of diversity and derailment.
Vision: A five-to-ten-year statement of what is over the horizon. Something so powerful that it motivates the team and brings it back to the course set by the practice after times of diversity and derailment.
 Core Values: A set of key behavior and decision-making principles, which are inviolate, and provide a safe haven whenever staff must make independent decisions for the good of the practice.
Core Values: A set of key behavior and decision-making principles, which are inviolate, and provide a safe haven whenever staff must make independent decisions for the good of the practice.
 Standards of Care: A consistent set of contemporary healthcare delivery commitments by all providers, that, while the client can waive, defer, appoint, or decide to do it, the practice cannot withhold the information of the needed level of care.
Standards of Care: A consistent set of contemporary healthcare delivery commitments by all providers, that, while the client can waive, defer, appoint, or decide to do it, the practice cannot withhold the information of the needed level of care.
 Mission Focus: An internal statement of to what and to where the practice standards apply for daily operations. For example, Client-centered patient advocacy to extend and enhance the quality and duration of an animal's life.
Mission Focus: An internal statement of to what and to where the practice standards apply for daily operations. For example, Client-centered patient advocacy to extend and enhance the quality and duration of an animal's life.
 Protocols: Operational systems on which the team can rely as constants, such as the AAHA Standards, and that no single person on the practice team can ignore or unilaterally change them.
Protocols: Operational systems on which the team can rely as constants, such as the AAHA Standards, and that no single person on the practice team can ignore or unilaterally change them.
 Case Management: Applying the professional skills and knowledge, such as Tilley's five-minute consult, of a specific doctor to a specific patient's needs, with the understanding that no single person on the practice team can ignore or unilaterally change the treatment plan, unless the case is transferred to that person by the attending doctor.
Case Management: Applying the professional skills and knowledge, such as Tilley's five-minute consult, of a specific doctor to a specific patient's needs, with the understanding that no single person on the practice team can ignore or unilaterally change the treatment plan, unless the case is transferred to that person by the attending doctor.
 Continuity of Care: The replicable outcome of the systems put in place for operational excellence in healthcare delivery, and kept in place by three concurrently operating systems:
Continuity of Care: The replicable outcome of the systems put in place for operational excellence in healthcare delivery, and kept in place by three concurrently operating systems:
 Zoned facility, with coordinators and operational staff teams accountable for zone excellence.
Zoned facility, with coordinators and operational staff teams accountable for zone excellence.
 Commitment of staff and doctors.
Commitment of staff and doctors.
 Management, including information technology, tracking to ensure consistently improving performance and outcomes.
Management, including information technology, tracking to ensure consistently improving performance and outcomes.
Concurrent with the above, there is an evolving necessity for medical record excellence. Medical record excellence means:
 There is a consistent system of legible data entry. For example, problem-oriented, with a systemized History-Exam-Assessment-Plan (H-E-A-P) or Subjective-Objective-Assessment-Plan (S-O-A-P) format.
There is a consistent system of legible data entry. For example, problem-oriented, with a systemized History-Exam-Assessment-Plan (H-E-A-P) or Subjective-Objective-Assessment-Plan (S-O-A-P) format.
 They are written in a timely manner. For example, in real time or before departing the practice for the day. This is done for the next person seeing the case, rather than just a memory jog for the attending provider.
They are written in a timely manner. For example, in real time or before departing the practice for the day. This is done for the next person seeing the case, rather than just a memory jog for the attending provider.
 They reflect contemporary diagnostics and professional knowledge, embracing the most current standards of care of the profession, rather than past practice paradigms or provider bias.
They reflect contemporary diagnostics and professional knowledge, embracing the most current standards of care of the profession, rather than past practice paradigms or provider bias.
 The staff can ensure a continuity of care with the information provided and maintain the patient's healthcare plan without any level of embarrassment to the initial provider, the next doctor, the practice, the staff, or even the client.
The staff can ensure a continuity of care with the information provided and maintain the patient's healthcare plan without any level of embarrassment to the initial provider, the next doctor, the practice, the staff, or even the client.
Click on the chart to see a larger view.
| Figure 2: Leadership Impact on Practice Operations | 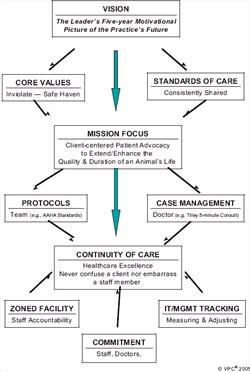
|
|
| |