Gregory K. Ogilvie, DVM, DACVIM (Specialties of Internal Medicine, Oncology)
Director, CVS Angel Care Cancer Center; President, Special Care Foundation for Companion Animals
San Marcos, CA, USA
Adapted from: Ogilvie GK, Moore AS. Managing the Veterinary Cancer Patient. Trenton NJ, Veterinary Learning Systems. 1995, 542 pages. Ogilvie GK, Moore AS. Feline Oncology: A Comprehensive Guide for Compassionate Care. Trenton NJ, Veterinary Learning Systems. 2002, 550 pages. Ogilvie GK, Moore AS. Managing the Canine Cancer Patient: A Practice Manual. Trenton NJ, Veterinary Learning Systems. 1-800-426-9119 http://veterinarylearningsystems.com/
A preoperative biopsy should be performed prior to definitive therapy if: 1) the results will alter the type of therapy to be employed, or 2) the results will influence the owner's willingness to treat.1
Guidelines1,2
 Biopsies do not negatively influence survival.
Biopsies do not negatively influence survival.
 A biopsy should be performed after consultation with the surgeon who will perform the surgery.
A biopsy should be performed after consultation with the surgeon who will perform the surgery.
 Obtain as large a sample as possible to enhance correct diagnosis by the pathologist.
Obtain as large a sample as possible to enhance correct diagnosis by the pathologist.
 The original architecture of the removed tissue should be maintained, therefore electrocautery or surgical instruments that crush or otherwise damage tissues should not be used.
The original architecture of the removed tissue should be maintained, therefore electrocautery or surgical instruments that crush or otherwise damage tissues should not be used.
 Ensure the tissue is adequately fixed in 10% buffered neutral formalin (1:10 parts fixative).
Ensure the tissue is adequately fixed in 10% buffered neutral formalin (1:10 parts fixative).
 Each biopsy should be placed into a separate, properly labeled container.
Each biopsy should be placed into a separate, properly labeled container.
 When possible, the entire lesion that has been resected and prepared properly should be submitted.
When possible, the entire lesion that has been resected and prepared properly should be submitted.
 Biopsies should be submitted to a highly qualified veterinary pathologist.
Biopsies should be submitted to a highly qualified veterinary pathologist.
Contraindications
In each case, the risks and benefits of the biopsy should be evaluated and clearly described to the owner. In most cases, the risks are minimal. Uncontrollable hemorrhage is the most common complication with all biopsy procedures except, perhaps with bone marrow aspiration and biopsy. Therefore, before each biopsy, hemostatic abnormalities should be identified and corrected. Infection at the local biopsy site or sepsis is an uncommon but serious problem that must be avoided by strict aseptic technique. Lastly, a biopsy should not be performed if it would put the success of a definitive procedure at risk.
Biopsy as a Prelude to Definitive Therapy
A palpable persistent mass or dominant nodule is the most common indication for biopsy as a prelude to definitive therapy.1-3 Because accuracy and sensitivity of diagnostic tests are improving, biopsies are being performed with increasing frequency to clarify the etiology of nonpalpable masses.
When developing a diagnostic strategy for a pet with cancer, the clinician must consider the subsequent management of the disease.3 The first step in management of most palpable lesions is fine-needle aspiration cytology. If the cytologic diagnosis strongly suggests a malignant condition, a definitive procedure such as surgery can then be planned. Fine needle aspiration cytology can also confirm the presence of a benign process, eliminating the need for further diagnostic steps. If fine-needle aspiration cytology is not definitive then an open biopsy should be performed, guided by the surgeon who will perform the indicated surgery. Prior to a biopsy procedure, standard staging procedures must be performed to identify any concurrent disease and to identify any clinically evident metastatic disease. Staging is accomplished by certain diagnostic tests that determine the extent of the neoplastic disorder. The staging scheme often differs for each neoplastic disease, but often includes a complete blood count, biochemical profile, urinalysis, chest radiographs and cytologic evaluation of regional lymph nodes.
| 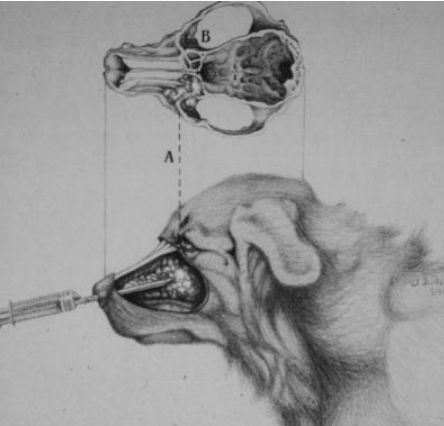
One contraindication for performing a biopsy is not knowing the anatomic sites that may result in serious problems. In this case, a nasal biopsy is obtained with a tube attached to a syringe. The cribriform plate (A) is the anatomic site of great importance when performing a nasal biopsy. |
|
| |
Skin Biopsy
A skin biopsy is essential to diagnose and evaluate potentially malignant skin conditions. Punch, incisional, excisional, and needle core biopsies are employed.1-3
Punch Biopsy1,3
Biopsy punches are disposable and available in diameters ranging from 2 mm to 6 mm. Generally, the larger biopsies are preferred so the pathologist has adequate tissue to make a histologic diagnosis. When possible, the junction between normal and abnormal tissue should be biopsied. Punch biopsies are usually inadequate to obtain tissue below the dermis; subcutaneous fat is rarely obtained in the average punch biopsy of the skin. Indication: Any dermal or epidermal lesion of unknown etiology.
Technique
1. The hair is clipped and the surgery site prepared with a surgical scrub.
2. Using a 25 gauge needle, approximately 2 to 3 mls of the local anesthetic agent lidocaine are injected around the lesion. It is important to not distort or disturb with lidocaine, the normal architecture of the tissue to be biopsied.
3. The biopsy area is scrubbed a final time after the lidocaine is injected.
4. The skin is stretched between the thumb and index finger.
5. The biopsy punch is placed at right angles to the skin surface.
6. The punch is rotated in one direction while at the same time firm downward pressure is applied until the subcutis is reached.
7. The punch is then angled almost parallel with the skin while still applying pressure along the long axis of the biopsy punch.
8. The punch is rotated to sever the base of the biopsied material.
9. The punch is removed.
10. The core of tissue is gently elevated with the point of a needle and the base severed with scalpel or iris scissors.
11. One to two sutures are placed to close the defect.
| 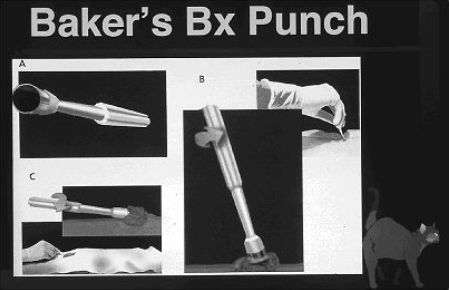
Baker's biopsy punches are easy to use by obtaining superficial biopsies. The instrument (A) is placed on the tumor and then rotated in one direction (B) until the desired depth is reached. Then the instrument is angled at a 45 degree angle while rotating the handle to "cut" off the base. |
|
| |
Incisional Biopsy1-3
In some cases, the incisional biopsy is preferred over a punch biopsy because larger sections of tissue can be obtained for histologic diagnosis. In addition, if the lesion is biopsied at the junction of the normal and abnormal tissue, a "wedge" of tissue is obtained that retains a larger section of the tissue's architecture. This allows the histopathologist to better see characteristics of malignancy, such as invasion of normal tissue.
Technique
1. The animal is placed under general anesthesia after routine screening tests have been performed to identify problems such as coagulopathies and metabolic disease.
2. The hair is clipped and the surgery site prepared with a surgical scrub.
3. After the region is draped, an elliptical or wedge incision is made at the margin of the normal and abnormal tissue. Care is taken to obtain adequate tissue and to ensure that a subsequent definitive surgery can successfully remove the tumor and the incisional biopsy incision.
4. Vessels going to and from the tissue to be biopsied are carefully identified and ligated.
5. The specimen is lifted and severed at the base with either scissors or a scalpel blade.
6. The incision is sutured for closure.
Excisional Biopsy1-3
An excisional biopsy should be performed when tissue is required for a histologic diagnosis, but the lesion must be small enough and in an anatomic location that allows for wide surgical removal without compromising the normal tissue around it. In general, an excisional biopsy is preceded with at least a fine needle aspirate cytology to give the surgeon as much information as possible about the characteristics of the tumor prior to removal. For example, a mast cell tumor or a soft tissue sarcoma would require wide surgical margins (2 to 3 cm), whereas a sebaceous cyst or sebaceous adenoma could be treated with smaller margins.
Technique
1. This biopsy is performed in the same manner as an incisional biopsy except the lesion is excised completely, with adequate margins.
Lymph Node Biopsy
Lymph node biopsy is often important in the diagnosis, staging and proper therapeutic management of the pet with cancer.1-3 A biopsy is often performed after fine-needle aspirate cytology suggests the presence of a disease. Despite the accuracy of fine-needle aspirate cytology in determining certain diseases such as lymphoma, mast cell tumors, and the presence of metastatic solid tumors, a histopathologic diagnosis is always recommended prior to initiation of therapy. In each case, adequate tissue must be obtained for histopathologic diagnosis and special stains, if indicated. When possible, the submandibular lymph nodes should be avoided, they often are reactive in the normal animal because they drain the oral cavity where the bacterial count is usually quite high. These reactive cells are sometimes misdiagnosed as neoplastic cells. If a carcinoma or a sarcoma is suspected, a biopsy should not be performed unless an overall plan for definitive therapy is made because the biopsy procedure can "seed" the operative field with tumor cells if the principle of en bloc dissection is violated. As with all biopsies, the surgeon who will perform the definitive surgery should be consulted prior to the biopsy to ensure that incisions are properly placed for a subsequent definitive procedure.
Needle Core Biopsy
Needle core biopsy is generally safe and quick, and can be performed on an awake cooperative patient.1 The histopathologic results are generally more accurate than fine needle aspirate cytology, but not as accurate as excisional biopsy.
Technique
The lymph node is grasped by an assistant and held firmly against the overlying skin, and the biopsy site is prepared as noted in steps 1 and 2 above. Then:
1. Approximately 2 to 3 mls of 2% lidocaine are injected under the skin overlying the enlarged lymph node.
2. Using a number 11 surgical blade, a stab incision is made in the skin to allow ease of entry of the needle core biopsy instrument.
3. The needle core biopsy instrument is advanced through the incision and into the capsule of the enlarged lymph node for subsequent biopsy.
4. At least 3 to 5 biopsies are taken of the lymph node through the same stab incision.
5. The needle biopsy specimens are fixed in 10% buffered formalin as described above. A separate container should be used for each lesion that is biopsied.
6. The stab incision is sutured only if indicated.
Bone Marrow Aspiration
Bone marrow aspiration and biopsy are essential procedures for determining cytologic and histologic abnormalities of the bone marrow that are caused by a wide variety of neoplastic, infectious, and myelodysplastic conditions.1-3 A bone marrow aspirate and biopsy are indicated when an abnormality in blood cell production is suspected or to appropriately stage an animal with a hematopoietic malignancy.
Bone marrow aspiration is performed to acquire a monolayer of cells for individual evaluation.1-3 To identify a wide variety of malignant and non-malignant disorders, Romanovsky (including Wright and Giemsa) stains are preferred. When the cytologic diagnosis of a cell type is not certain, additional special stains can be used including myeloperoxidase, Sudan black, and periodic acid Schiff. Bone marrow biopsies are beneficial for determining bone marrow cellularity, the presence and extent of fibrosis or granulomatous conditions, and the presence of non-hematopoietic malignancies.
| 
Spring loaded "automatic" needle core biopsy instruments are great for obtaining lymph node or other tissue samples with a local block and lidocaine anesthesia. |
|
| |
Technique1-3
1. The hair is clipped and the bone marrow aspiration site is prepared with a surgical scrub. Preferred sites and patient positioning include: dorsocranial or lateral aspects of iliac crest (patient is sternal); greater trochanter of the femur (patient is in lateral recumbency); greater tubercle of the proximal aspect of the head of the humerus (patient is in lateral recumbency).
2. Using a 25 gauge needle, approximately 2 to 3 mls of the local anesthetic agent, lidocaine, are injected in and around the site where the bone marrow needle is to be introduced. Care is taken to deposit lidocaine in and around all of the tissues that extend from the skin to the bone.
3. The biopsy area is scrubbed a final time after the lidocaine is injected. A surgical drape can be applied for sterility.
4. The bone marrow site is identified, the skin is stretched between the thumb and index finger, and a small stab incision is made with a number 11 surgical blade in the area blocked with lidocaine.
5. The bone marrow needle with the stylette in place is advanced through the stab incision in the skin, subcutaneous tissue, and muscle down to the bone. It is crucial to keep the stylette in place because it has a tendency to back out during the procedure. A 1 to 1.5 inch long, 16 gauge Illinois or Rosenthal bone marrow needle is preferred for dogs, and a 1 inch long, 18 gauge Illinois or Rosenthal needle is preferred for the cat. After a sample is obtained for cytologic evaluation, if a biopsy is required, a Jamshidi needle is utilized.
6. With the stylette is place, the bone marrow needle is advanced into the bone using a corkscrew motion. The instrument should not be allowed to wobble and the instrument should be fixed firmly into bone like a nail that has been securely hammered into wood. When the needle is firmly fixed in the bone, the stylette is removed and the syringe is affixed. Many clinical pathologists suggest rinsing the syringe and bone marrow needle with EDTA before the procedure to reduce clotting of the bone marrow sample.
7. The bone marrow sample is then aspirated briskly into the 12 ml syringe; usually 1 ml is adequate. The aspiration may be accompanied with a few seconds of pain, but this cannot be prevented.
8. If a sample is not obtained, the stylette is replaced in the bone marrow needle and the instrument is then advanced further into the bone for a second attempt at aspirating marrow contents.
9. Once marrow has been obtained, smears are prepared. This can be done a number of ways.
| 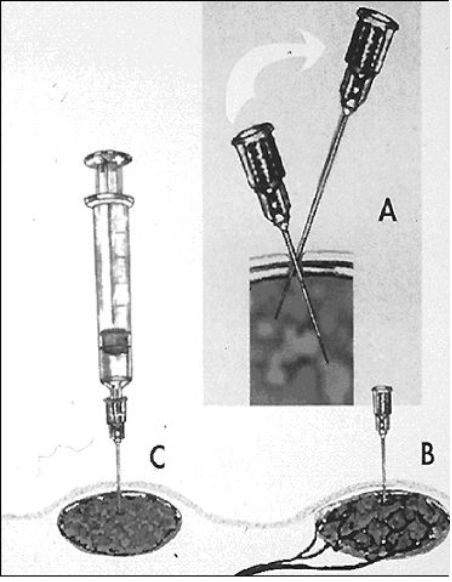
Fine needle aspiration without (A and B above) or without (C above) the syringe attached to the needle is an important clinical tool for obtaining cells for a diagnosis. |
|
| |
References
1. Withrow SJ: Biopsy Principles, in Withrow SJ, MacEwen EG (eds): Clinical Veterinary Oncology, Philadelphia, JB Lippincott Co. 1989, pp 53-57.
2. Morrison WB, Hamilton TA, Hahn KA, Richardson RC, Janas W: Diagnosis of Neoplasia. In Slatter D (ed): Textbook of Small Animal Surgery (2nd ed), Philadelphia, WB Saunders Co, 1993, pp 2036-2048.
3. Avis F: Lymph Node Biopsy, in Wittes RE (ed) Manual of Oncologic Therapeutics 1991/1992. Philadelphia, JB Lippincott Co. 1991, pp 8-9.